- Article
- Source: Campus Sanofi
- Aug 6, 2025
The burden and Risk of Exacerbations in COPD according to Dr. Surya Bhatt
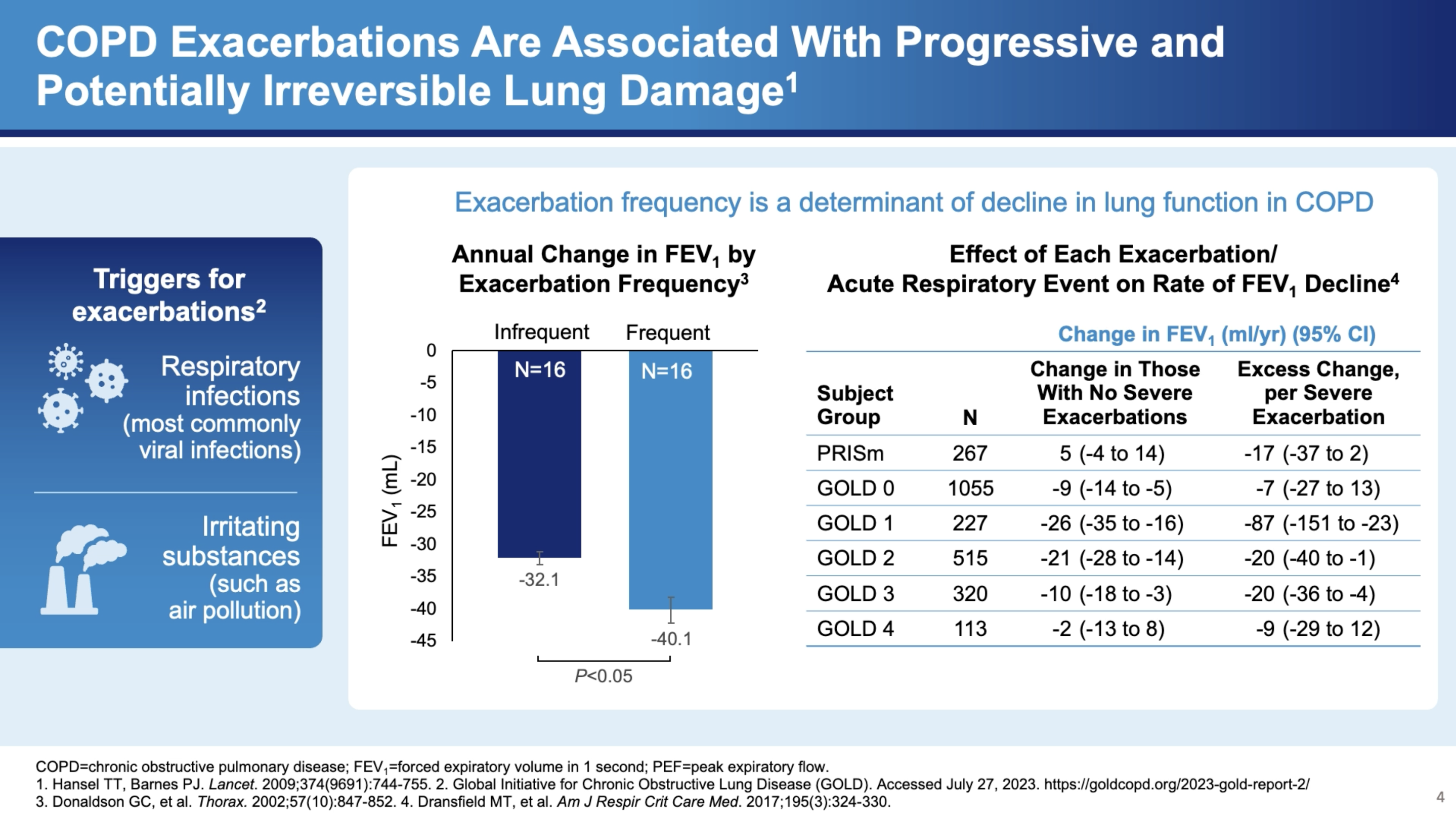
My name is Surya Bhatt. I'm a professor of medicine at the University of Alabama at Birmingham, and I'm a COPD researcher. This talk is sponsored by Sanofi and Regeneron, and you won't get any CME credit. One of the other things that's very important in COPD is acute exacerbations. And these are not just an inconvenience but are associated with significant disease progression. Now there's plenty of data to suggest that these exacerbations are associated with lung function decline. They're commonly caused by infections such as viruses and bacterial infections sometimes due to environmental pollution and occupational exposures. Regardless of the cause, the severity is determined by where they're treated, which is not ideal. But if they manage to adjust steroids and antibiotics at home, that classifies as a moderate exacerbation. But if it's severe enough to end up in the hospital, and then that causes a severe exacerbation and people will suffer from exacerbations, have a faster rate of lung function decline than those who do not have exacerbations at all. And here on the right is data from the COPD gene study where they looked at the FEV one decline by exacerbation or the frequency of exacerbations.
And especially for severe exacerbations and especially for those with milder disease who have more lung function to lose the effect can be quite dramatic. The FEV even decline can be up to 87mm for a severe exacerbation in world stage one, for example. And as you can imagine, if you get 4 or 5 exacerbations, you can lose up to a half a meter of fev1 over the next 4 to 5 years. The severe exacerbations appear to be sentinel events in the course of the COPD patients. When somebody gets a first exacerbation it seems like it begets more exacerbations. In a retrospective study by Sammy Sosa of about 75,000 patients in Canada. He modeled the severe exacerbation frequency and found that the usual median interval between a first and a second exacerbation is about five and a half years, and then the exacerbations happen at progressively shorter intervals to the point that by about the 10th exacerbation the median interval is about four months. So you can imagine a patient within a few years settling into a pattern of 3 to 4 exacerbations needing hospitalization in a single year.
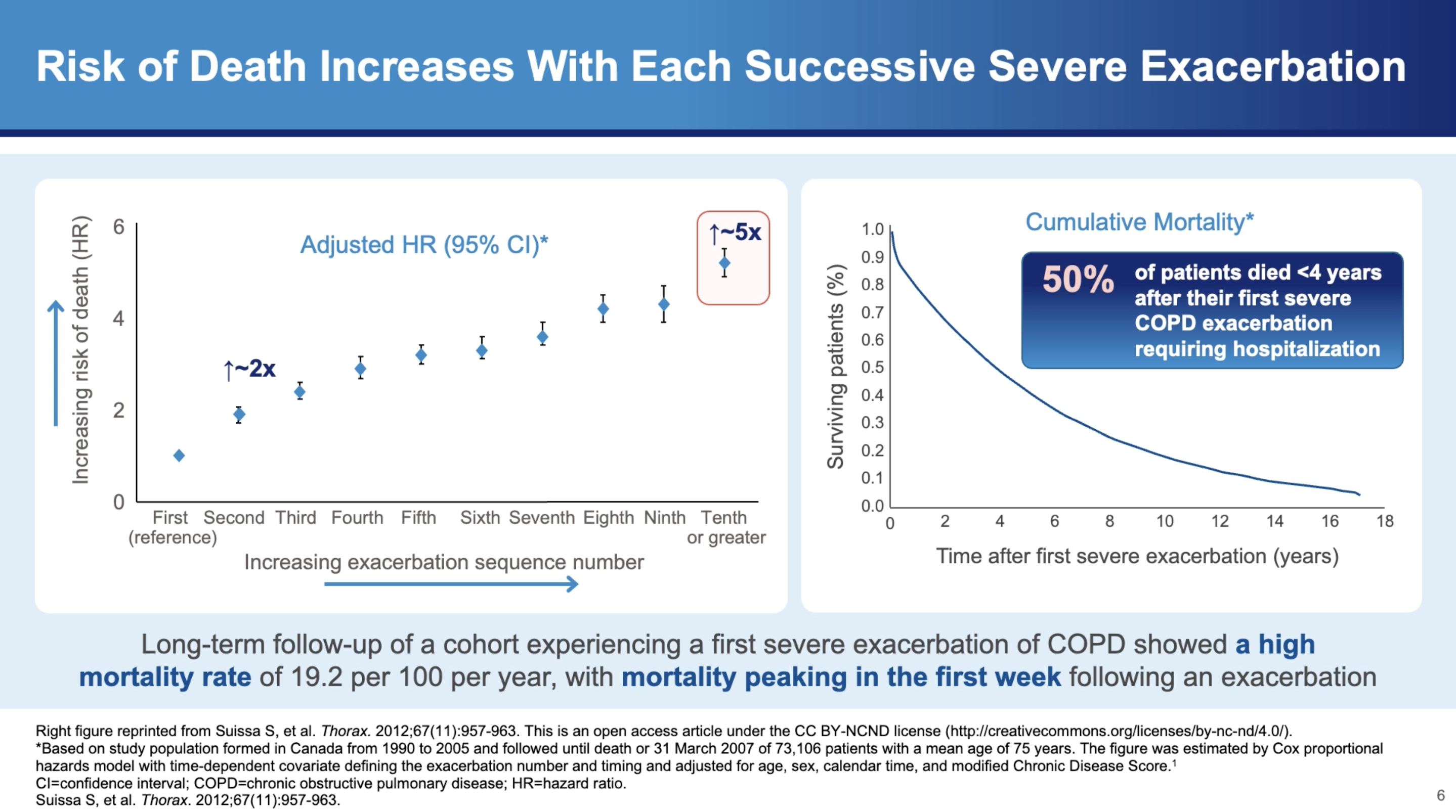
And this is not without consequence. These kind of exacerbations can have an effect on mortality. The hazards of mortality is about twice. If you get two severe exacerbations as opposed to one severe exacerbation. And the hazards of mortality is five fold. If you get ten exacerbations as opposed to one severe exacerbation. So there's almost a monotonic increase in the hazards with increasing severe exacerbation frequency. And the curve on the right shows your risk of dying after a single severe exacerbation requiring hospitalization. So the mortality within one year is about 25%, and the mortality within four years after discharge after the first severe exacerbation is 50%.
What is COPD?
COPD is a chronic inflammatory lung disease that causes obstructed airflow from the lungs.1 Symptoms include breathing difficulty, cough, mucus (sputum) production, and wheezing. It is typically caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. Individuals with COPD are at increased risk of developing heart disease, lung cancer, and a variety of other conditions.1
The Critical Role of Exacerbations in COPD Progression
Dr. Bhatt emphasizes that acute exacerbations of COPD are not merely inconveniences but are pivotal events that significantly influence the course of the disease. "One of the other things that's very important in COPD is acute exacerbations. And these are not just an inconvenience but are associated with significant disease progression," he states. Exacerbations are typically triggered by infections such as viruses and bacterial infections or by environmental pollution and occupational exposures.1
Impact on Lung Function
Exacerbations have a profound impact on lung function, with data suggesting a link between exacerbations and accelerated lung function decline.1 Dr. Bhatt notes, "There's plenty of data to suggest that these exacerbations are associated with lung function decline." This decline is more severe in the case of frequent exacerbations. For instance, he cites the COPD Gene study, which shows how the frequency of exacerbations correlates with the rate of FEV1 decline—a measure of lung function.2
Severity and Treatment1
The severity of exacerbations can vary, significantly affecting treatment approaches and outcomes.1 "But if they manage to adjust steroids and antibiotics at home, that classifies as a moderate exacerbation. But if it's severe enough to end up in the hospital, then that causes a severe exacerbation," explains Dr. Bhatt. The distinction between moderate and severe exacerbations is crucial as it determines the immediate treatment protocol and the long-term management strategy.
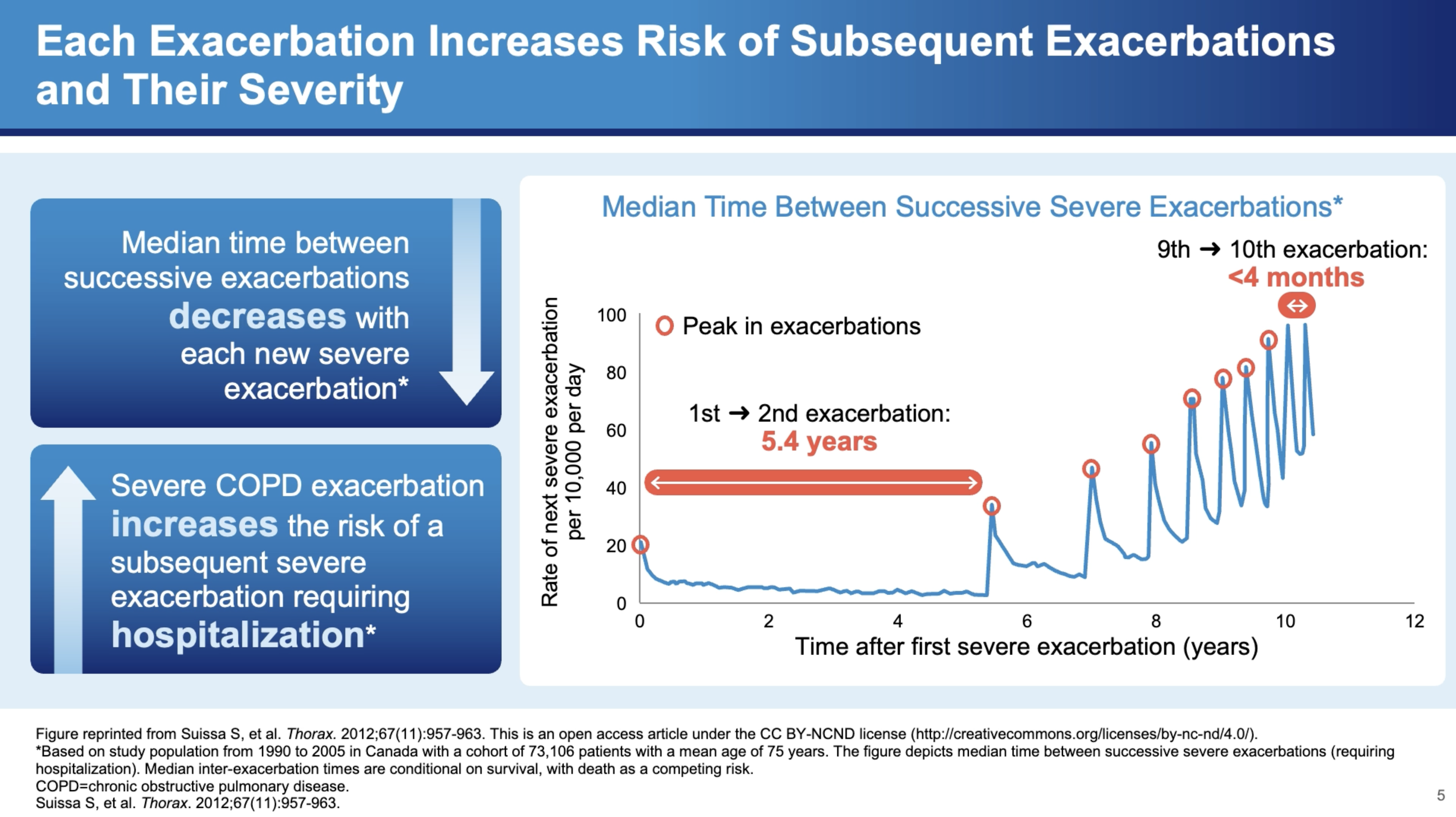
The Cascading Effects of Severe Exacerbations
Severe exacerbations are particularly concerning due to their cascading effects on health. Dr. Bhatt discusses a study by Samy Suissa, which modeled severe exacerbation frequency among approximately 75,000 patients in Canada.3 The study found that the interval between exacerbations tends to decrease over time, indicating a worsening pattern of the disease. "When somebody gets a first exacerbation, it seems like it begets more exacerbations," he explains.
Mortality Risks
The mortality risks associated with severe exacerbations are stark. Dr. Bhatt highlights, "The hazards of mortality is about twice if you get two severe exacerbations as opposed to one severe exacerbation. And the hazards of mortality is fivefold if you get ten exacerbations as opposed to one severe exacerbation." Furthermore, the risk of dying within one year of a severe exacerbation requiring hospitalization is about 25%, which increases to 50% within four years after discharge.
In Summary
The insights provided by Dr. Surya Bhatt illuminate the severe implications of COPD exacerbations. Understanding the triggers, frequency, and severity of these exacerbations is crucial for managing COPD effectively. As research continues to evolve, it is essential for healthcare providers to stay informed about the best practices for treating and managing exacerbations to improve the quality of life for COPD patients. Additionally, preventative strategies, including smoking cessation and reducing exposure to pollutants, remain key components of COPD management. Through a comprehensive approach that includes both prevention and effective exacerbation management, the impact of COPD can be significantly mitigated.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Accessed July 31, 2025. https://goldcopd.org/2025-gold-report//.
- Dransfield MT, Kunisaki KM, Strand MJ, Anzueto A, Bhatt SP, Bowler RP, Criner GJ, Curtis JL, Hanania NA, Nath H, Putcha N, Roark SE, Wan ES, Washko GR, Wells JM, Wendt CH, Make BJ; COPDGene Investigators. Acute Exacerbations and Lung Function Loss in Smokers with and without Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2017 Feb 1;195(3):324-330.
- Suissa S, Dell'Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012 Nov;67(11):957-63.
MAT-GLB-2400917-V-1.0