- Article
- Source: Campus Sanofi
- Apr 30, 2024
An Overview of the impact of Type 2 Inflammation in COPD: Insights from Dr. Surya Bhatt


My name is Surya Bhatt. I'm a professor of Medicine at the University of Alabama at Birmingham and I'm a COPD researcher.
This talk is sponsored by Sanofi and Regeneron and you won't get any (CME) credit. In response to any kind of insult. For example, cigarette smoke, viral infections, bacterial infections, pollution, there is some element of epithelial injury and epithelial damage. And the first response to this usually is once there is enough epithelial damage, there is release of damage associated molecular patterns or (DAMPs) which are now perhaps more popularly called alarmins and these are IL-33, IL-25 and TSLP or thymic stromal lymphopoietin. So all these can be released and they all have specific roles in terms of furthering inflammation. And IL-33 is perhaps best understood and some people consider it the master inflammation switch where once it's activated, it stays activated for a long time. It promotes both type 1 and type 3 inflammation as well as type 2 inflammation.
The traditional thinking has been that the prime driver of type two inflammation is IL-5, which causes eosinophilic inflammation. But now we understand that both IL-4 and IL-13 are important in driving type 2 inflammation. And here's a list of all the things that they can do. lL-4 and IL-13:
Can both cause epithelial barrier disruption.
They can cause B cell class switching and enhance an increased production of IgE
They can cause mast cell degranulation
They can cause basophil degranulation
And also eosinophilic inflammation just like IL-5.
They can also result in goblet cell hyperplasia and mucus production especially IL-13.
And as a consequence of these, they can cause significant airway remodeling as well as alveolar destruction.
IL-4 and IL-13 levels are also elevated during an acute exacerbation as opposed to in the stable state or patients without COPD. So this is also important to note that these pathways are activated in patients with acute exacerbation of COPD and they present and important in COPD.
And then, you know, we all know that there's been a lot of understanding of mucin and mucus production in COPD. And one of the prime drivers of that is MUC5A and IL-4 can induce increased expression of MUC5AC in human epithelial cells. And there's also a dose dependent response almost of IL-13 on MUC5A as well as increased mucus production. So, especially IL-13 has been found to be an important driver of mucus production in patients with COPD.
Understanding COPD and Inflammation Pathways
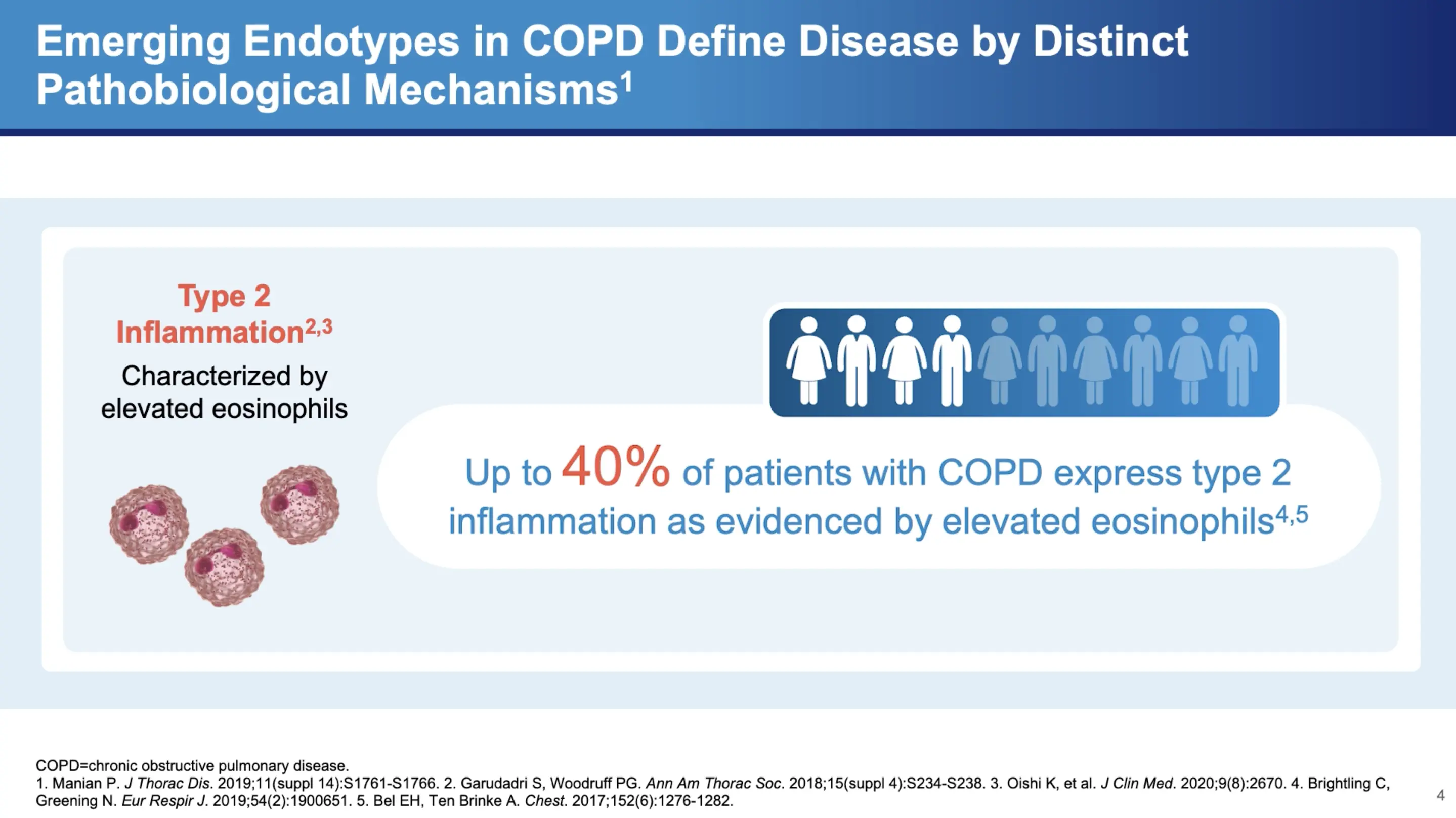
COPD has historically been viewed through the lens of neutrophilic inflammation, driven primarily by the DH1 and DH17 pathways. However, Dr. Bhatt highlights a shift in understanding, noting that "there's increasing recognition that Type 2 inflammation may actually play a role in COPD." This inflammation is not as straightforward to detect, with varying degrees of presence in the patient population. "It's between 20 to 40 percent of patients seem to have some evidence of Type 2 inflammation," Dr. Bhatt explains.
Diagnostic Markers of Type 2 Inflammation
One of the key markers for detecting Type 2 inflammation is the eosinophil count in the blood. Dr. Bhatt points out the diagnostic value of this marker: "It correlates relatively well with eosinophilic inflammation in the lungs and it's more likely to be specific than sensitive." This means that a high eosinophil count can be a reliable indicator of Type 2 inflammatory activity within the lungs. However, he also cautions that fluctuating eosinophil levels can complicate the diagnosis, stating, "if you don't find it, that doesn't mean they don't have Type 2 inflammation."
Clinical Implications of Type 2 Inflammation in COPD
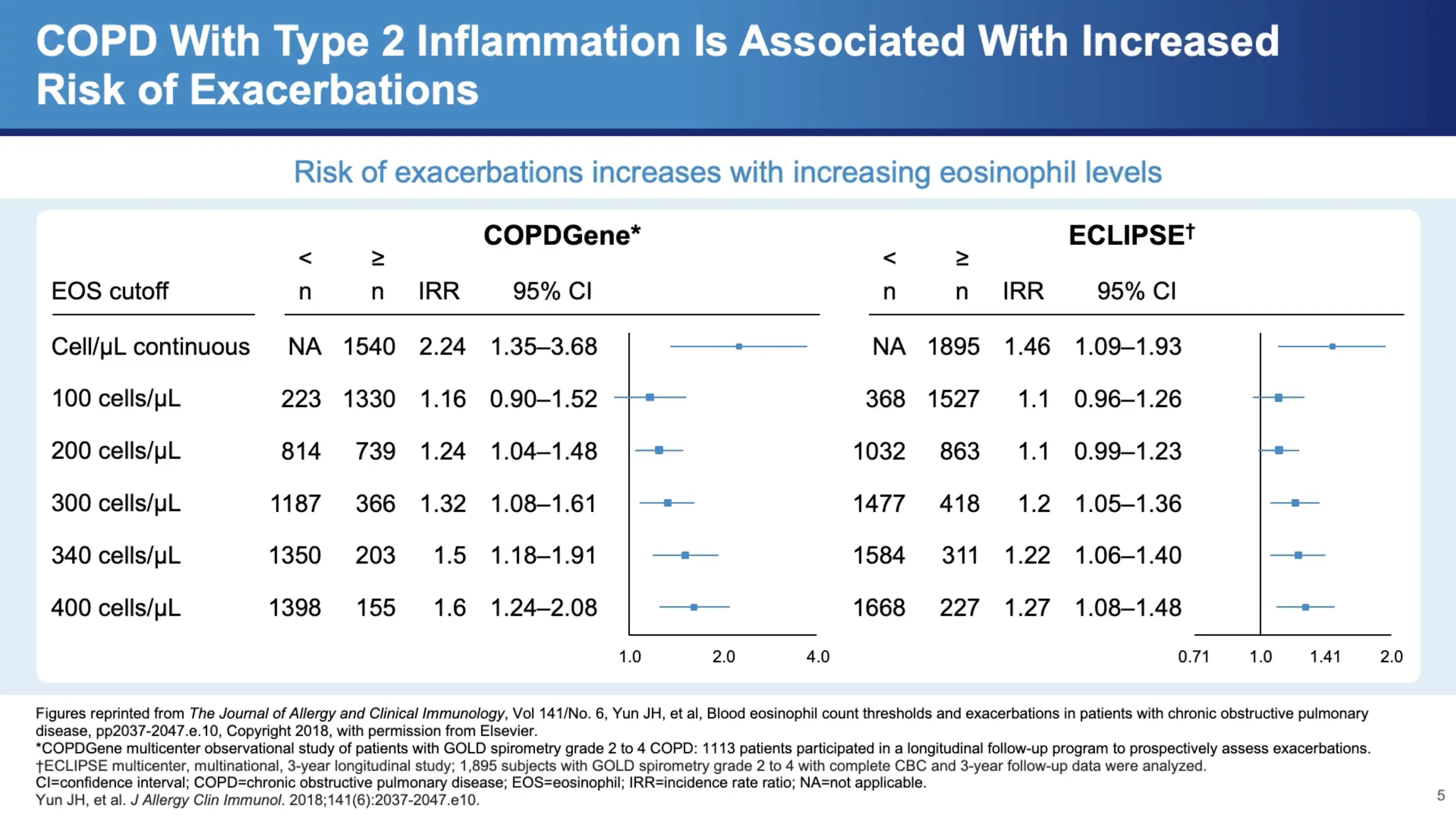
Dr. Bhatt refers to data from significant studies such as COPD Gene and Eclipse, which show a clear correlation between eosinophil counts and exacerbation frequency in COPD patients. "There's almost a monotonic increase in the frequency of exacerbations with increasing eosinophil count," he notes, highlighting the clinical relevance of these findings. Notably, around 300 cells per microliter marks a significant increase in exacerbation frequency, which continues to rise with higher counts.
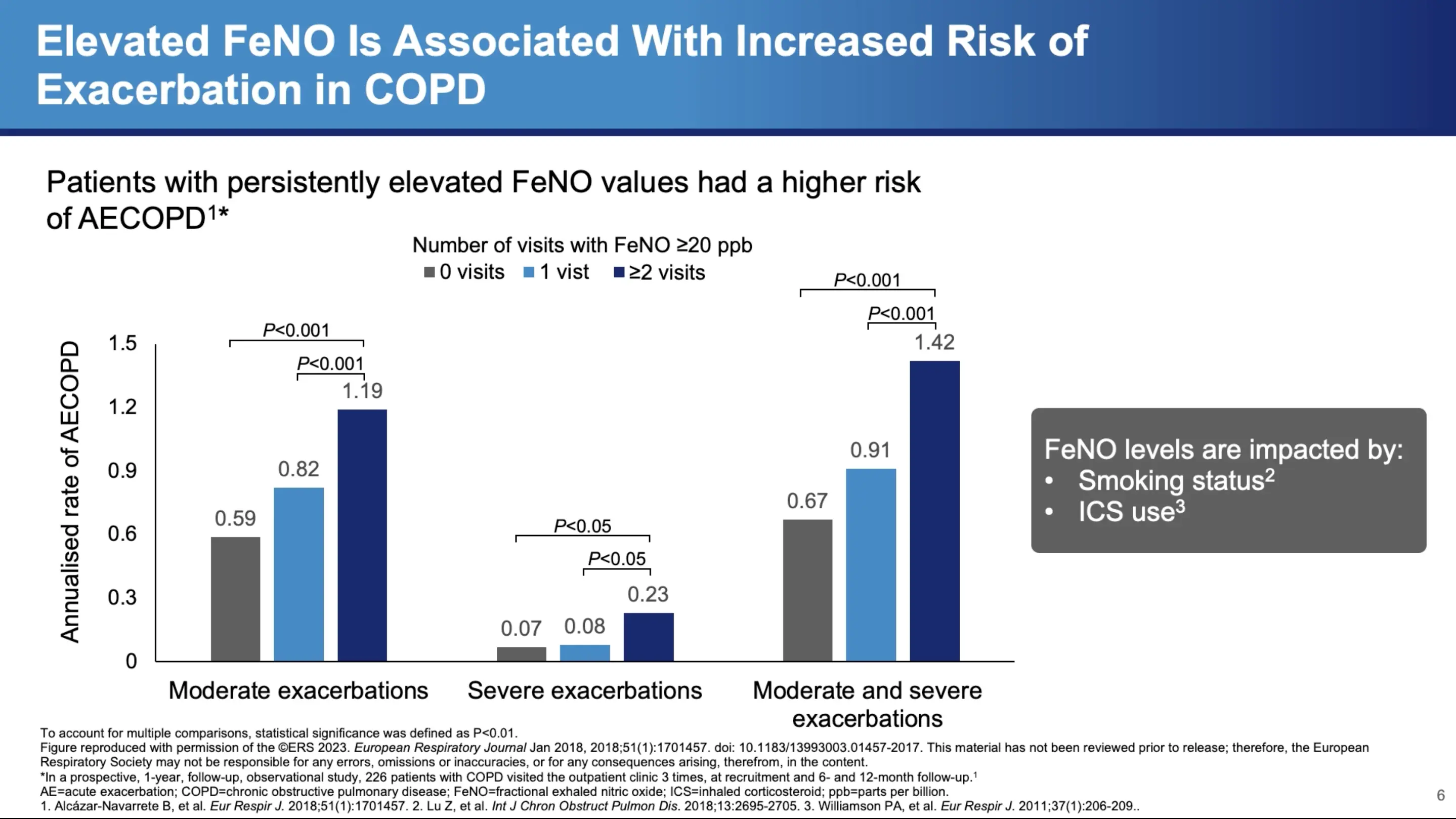
Additionally, other diagnostic tools like fractional exhaled nitric oxide (FeNO) can offer insights into Type 2 inflammation. Dr. Bhatt discusses a study involving 220 patients, which found that varying levels of FeNO were associated with different exacerbation frequencies. Those with persistently elevated FeNO levels showed a continuous increase in exacerbations, suggesting ongoing Type 2 inflammation.
Prognostic Value of Type 2 Inflammation
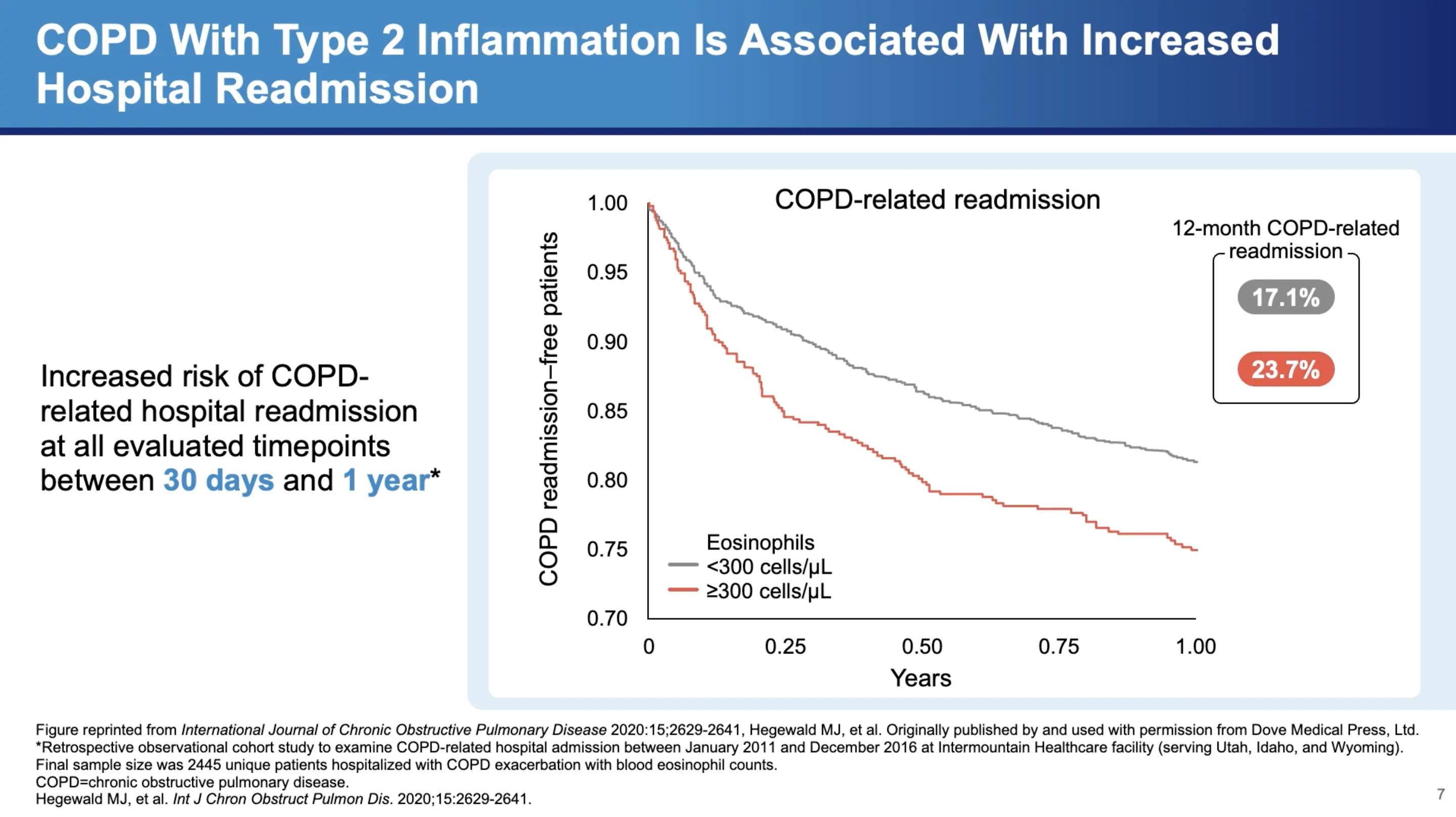
Type 2 inflammation not only correlates with exacerbation frequency but also has implications for hospital readmissions. Dr. Bhatt cites a retrospective study of almost 2,500 patients from an administrative database, revealing that "high eosinophils, defined as greater than 300 cells per microliter, was associated with a higher COPD-related readmission at 30 days as well as at 52 weeks." This finding underscores the importance of monitoring eosinophil levels for predicting both moderate and severe exacerbations, and potentially tailoring treatment strategies to reduce hospital readmissions.
In Summary
Dr. Surya Bhatt's insights into Type 2 inflammation in COPD highlight a significant shift in understanding and managing this complex disease. Recognizing the role of Type 2 inflammation could lead to more personalized treatment approaches, potentially improving outcomes for a substantial subset of COPD patients. As research continues to evolve, pulmonologists and other healthcare providers must stay informed about these developments to optimize care for their patients with COPD.
In summarizing the impact of these findings, Dr. Bhatt emphasizes the need for continued research and awareness, "I think we need to keep looking," he asserts, pointing towards a future where COPD treatment may become more targeted and effective based on individual inflammatory profiles. This approach could revolutionize the management of COPD, making it not just a matter of managing symptoms but potentially altering the disease course for many patients.
References
- Gandhi NA, Bennett BL, Graham NMH, et al. Targeting key proximal drivers of type 2 inflammation in disease. Nat Rev Drug Discov. 2016;15(1):35-50.
- Yousuf A, Ibrahim W, Greening NJ, et al. T2 Biologics for Chronic Obstructive Pulmonary Disease. J Allergy Clin Immunol Pract. 2019;7(5):1405-1416.
- Aghapour M, Raee P, Moghaddam SJ, et al. Airway Epithelial Barrier Dysfunction in Chronic Obstructive Pulmonary Disease: Role of Cigarette Smoke Exposure. Am J Respir Cell Mol Biol. 2018;58(2):157-169.
- Barnes JP. Inflammatory endotypes in COPD. Allergy. 2019;74(7):1249-1256.
- Wang Z, Bafadhel M, Haldar K, et al. Lung microbiome dynamics in COPD exacerbations. Eur Respir J. 2016;47(4):1082-1092.
- Smithgall MD, Comeau MR, Yoon BRP, et al. IL-33 amplifies both Th1- and Th2-type responses through its activity on human basophils, allergen-reactive Th2 cells, iNKT and NK cells. Int Immunol. 2008;20(8):1019-1030.
- Senra L, Mylonas A, Kavanagh RD, et al. IL-17E (IL-25) enhances innate immune responses during skin inflammation. J Invest Dermatol. 2019;139(8):1732-1742.
- Linden D, Guo-Parke H, Coyle PV, et al. Respiratory viral infection: a potential “missing link” in the pathogenesis of COPD. Eur Respir Rev. 2019; 28(151):180063.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Accessed July 27, 2023. https://goldcopd.org/2023-gold-report-2/.
- Calderon AA, Dimond C, Choy DF, et al. Targeting interleukin-33 and thymic stromal lymphopoietin pathways for novel pulmonary therapeutics in asthma and COPD. Eur Respir Rev. 2023;32(167):220144.
- Kurokawa M, Matsukura S, Kawaguchi M, et al. Interleukin-33-activated dendritic cells induce the production of thymus and activation-regulated chemokine and macrophage-derived chemokine. Int Arch Allergy Immunol. 2013;161(Suppl 2):52-57.
- Griesenauer B, Paczesny S. The ST2/IL-33 axis in immune cells during inflammatory diseases. Front Immunol. 2017;8:475.
- Borowczyk J, Shutova M, Brembilla NC, et al. IL-25 (IL-17E) in epithelial immunology and pathophysiology. J Allergy Clin Immunol. 2021;148(1):40-52.
- Claudio E, Wang H, Kamenyeva O, et al. IL-25 orchestrates activation of Th cells via conventional dendritic cells in tissue to exacerbate chronic house dust mite–induced asthma pathology. J Immunol. 2019;203(8)2319-2327.
- Kotlyarov S. Involvement of the innate immune system in the pathogenesis of chronic obstructive pulmonary disease. Int J Mol Sci. 2022;23(2):985.
- Gandhi NA, Pirozzi G, Graham NMH. Commonality of the IL-4/IL-13 pathway in atopic diseases. Expert Rev Clin Immunol. 2017;13(5):425-437.
- Saatian B, Rezaee F, Desando S, et al. Interleukin-4 and interleukin-13 cause barrier dysfunction in human airway epithelial cells. Tissue Barriers. 2013;1(2):e24333.
- Zheng T, Zhu Z, Wang Z, et al. Inducible targeting of IL-13 to the adult lung causes matrix metalloproteinase- and cathepsin-dependent emphysema. J Clin Invest. 2000;106(9):1081-1093.
- Zhu Z, Homer RJ, Wang Z, et al. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest. 1999;103(6):779-788.
- Alevy YG, Patel AC, Romero AG, et al. IL-13-induced airway mucus production is attenuated by MAPK13 inhibition. J Clin Invest. 2012;122(12):4555-4568.
- Wang X, Xu C, Ji J, et al. IL-4/IL-13 upregulates Sonic hedgehog expression to induce allergic airway epithelial remodeling. Am J Physiol Lung Cell Mol Physiol. 2020;318(5):L888-L899.
- Cooper PR, Poll CT, Barnes PJ, et al. Involvement of IL-13 in tobacco smoke-induced changes in the structure and function of rat intrapulmonary airways. Am J Respir Cell Mol Biol. 2010;43(2):220-226.
- Doyle AD, Mukherjee M, LeSuer WE, et al. Eosinophil-derived IL-13 promotes emphysema. Eur Respir J. 2019;53(5):1801291.
- Sun J, Liu T, Yan Y, et al. The role of Th1/Th2 cytokines played in regulation of specific CD4+ Th1 cell conversion and activation during inflammatory reaction of chronic obstructive pulmonary disease. Scand J Immunol. 2018;88(1):e12674.
- Kim CH, Kim KE, Yoon JH, et al. Upregulation of MUC5AC gene expression by IL-4 through CREB in Human airway epithelial cells. J Cell Biochem. 2009;108(4):974-981.
- Yu H, Li Q, Kolosov VP, et al. Interleukin-13 induces mucin 5AC production involving STAT6/SPDEF in human airway epithelial cells. Cell Commun Adhes. 2010;17(4-6):83-92.
MAT-GLB-2400917-V-1.0