- Article
- Source: Campus Sanofi
- Aug 14, 2024
COPD vs asthma: Learn the difference

The overlapping signs and symptoms of COPD and asthma can make it challenging to distinguish between the two conditions.2 Certain patient groups pose a challenge for accurate diagnose of COPD due to confounding clinical features.2
COPD and asthma are obstructive lung disorders with distinct epidemiological features and pathophysiology. 3,4 Furthermore, these two conditions have different guideline-recommended management strategies and treatment goals.4 Thus, there is a need to make a clear distinction between the two conditions for accurate diagnosis and optimal management.
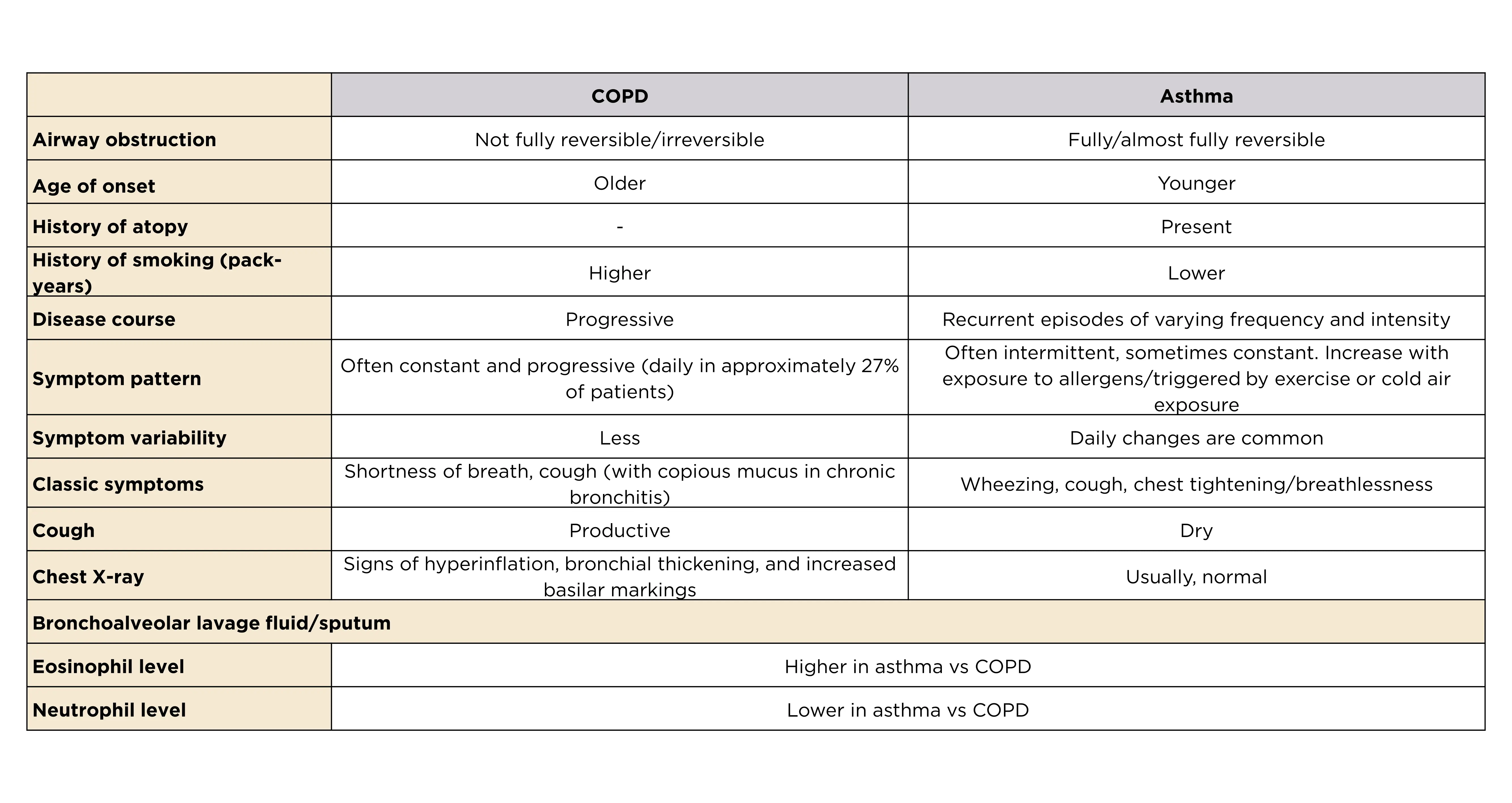
COPD is a chronic, usually progressive disease, typically associated with smoking and diagnosed in middle and relatively older age group (>40 years old).2,3 It is characterized by airflow obstruction that is not fully reversible or irreversible.2,4
On the contrary, asthma is characterized by bronchial hyperresponsiveness, inflammation of airways, and airflow obstruction.2 Typically, asthma is an allergic disorder2 and associated with atopy.4 It presents during childhood, though it can be diagnosed in adulthood as well.3
Distinguishing between COPD and asthma4
Type 2 inflammation in COPD and asthma
Both COPD and asthma are associated with chronic inflammation of the respiratory tract.5 Although cells and mediators involved in inflammation are different between the two disease entities, some patients with COPD have an inflammatory pattern (type 2 inflammation) similar to that in asthma.5,6
Type 2 inflammation, associated with eosinophilic inflammation, is characteristic of asthma, while COPD is mostly associated with neutrophilic inflammation.4,7 However, evidence has suggested that increased eosinophil count in the airways and type 2 inflammation may be present in a subgroup of patients with COPD as well, even without coexisting asthma.6,7 Notably, type 2 inflammation is associated with increased risk of exacerbations in asthma and in moderate to severe COPD.8
Click here to gather more insights from Dr. Surya Bhatt on the impact of type 2 inflammation in COPD.
Click here to read more about the role of type 2 inflammation in COPD exacerbations.
COPD and asthma overlap
The Global Initiative for Asthma (GINA) 2024 strategy report terms COPD and asthma overlap as a simple description for patients with symptoms of both COPD and asthma.1 The Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2024 report emphasizes that these two conditions are separate but does acknowledge that they may coexist.5 Asthma reportedly coexists in approximately 27% of patients with COPD.3 In case of a concurrent diagnosis, 2024 GOLD report recommends managing the disease using the asthma guidelines.5
Characteristics of COPD and asthma overlap vs COPD alone3

Bronchodilator response: COPD vs asthma
Abnormal levels of forced expiratory volume in 1 minute (FEV1) and forced vital capacity (FVC) are suggestive of airflow obstruction.4 Pre-bronchodilator spirometry can be used for initial assessment of airflow obstruction in symptomatic patients.5 Post-bronchodilator spirometry is needed for COPD diagnosis and assessment; FEV1/FVC ratio of <0.7 is considered diagnostic for COPD.5 Post-bronchodilator spirometry can also be useful in distinguishing between classical asthma presentation and COPD.4 Airflow obstruction is often fully reversible in classical asthma, while it is irreversible or partially reversible in COPD.4 However, the degree of reversibility may vary in an individual patient and coexistence of COPD and asthma may confound bronchodilator response.4,5 Therefore, post-bronchodilator spirometry should not be considered as the only criterion for differentiating COPD from asthma.4
Click here to know about the key tools to measure COPD severity.
COPD and asthma treatment guidelines
COPD management5
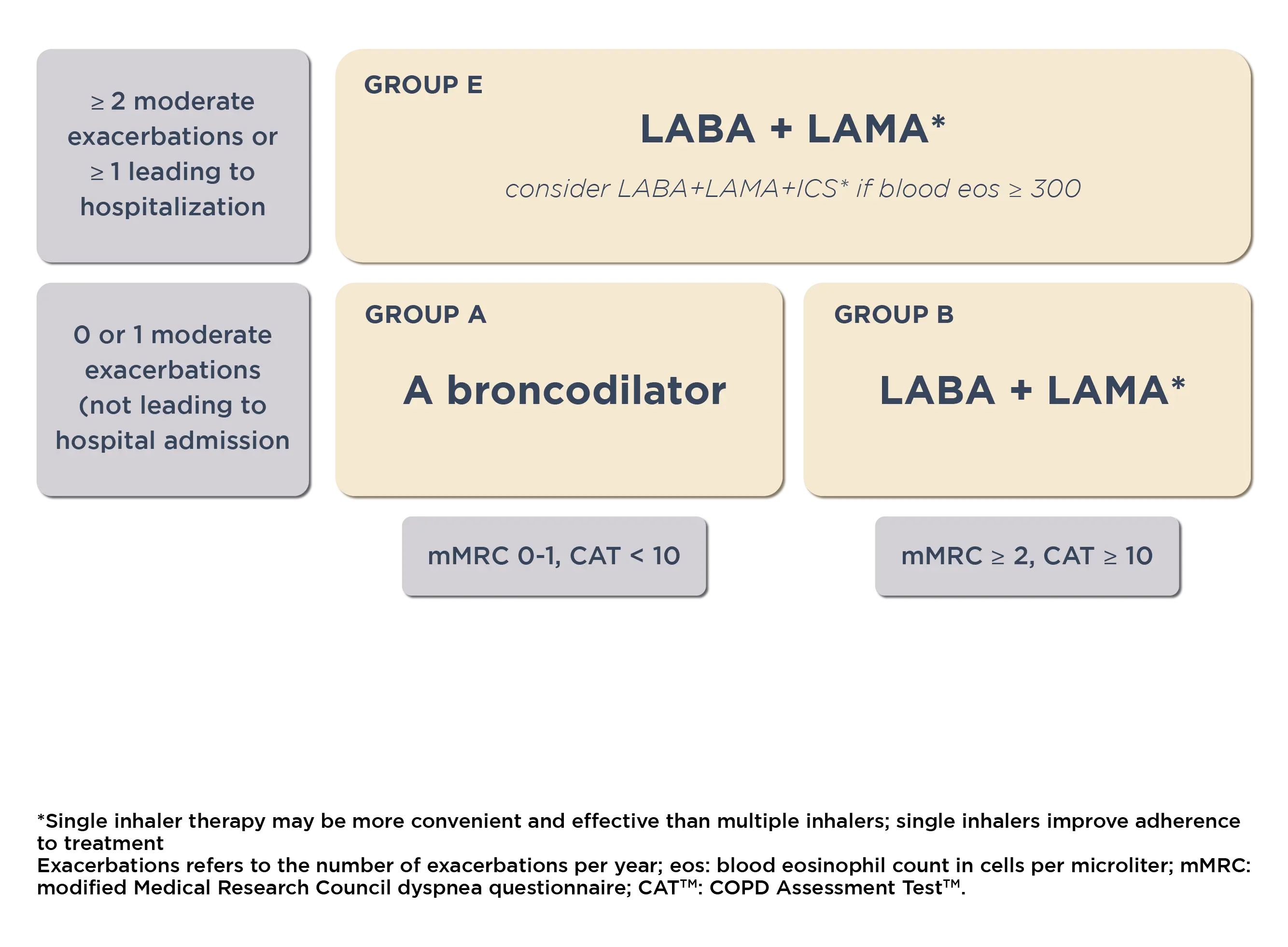
The treatment goals of COPD exacerbations are to reduce symptoms and future risk of exacerbations. 2024 GOLD report proposes a tailored approach for COPD management, based on the severity of symptoms and exacerbation risk.
Treatment can be escalated/de-escalated based upon predominant symptoms (treatable traits) of breathlessness and exercise limitation, and the continued occurrence of exacerbations whilst on maintenance therapy.
Click here to read the 2024 GOLD recommendations for COPD management.
Initial pharmacological treatment for COPD5
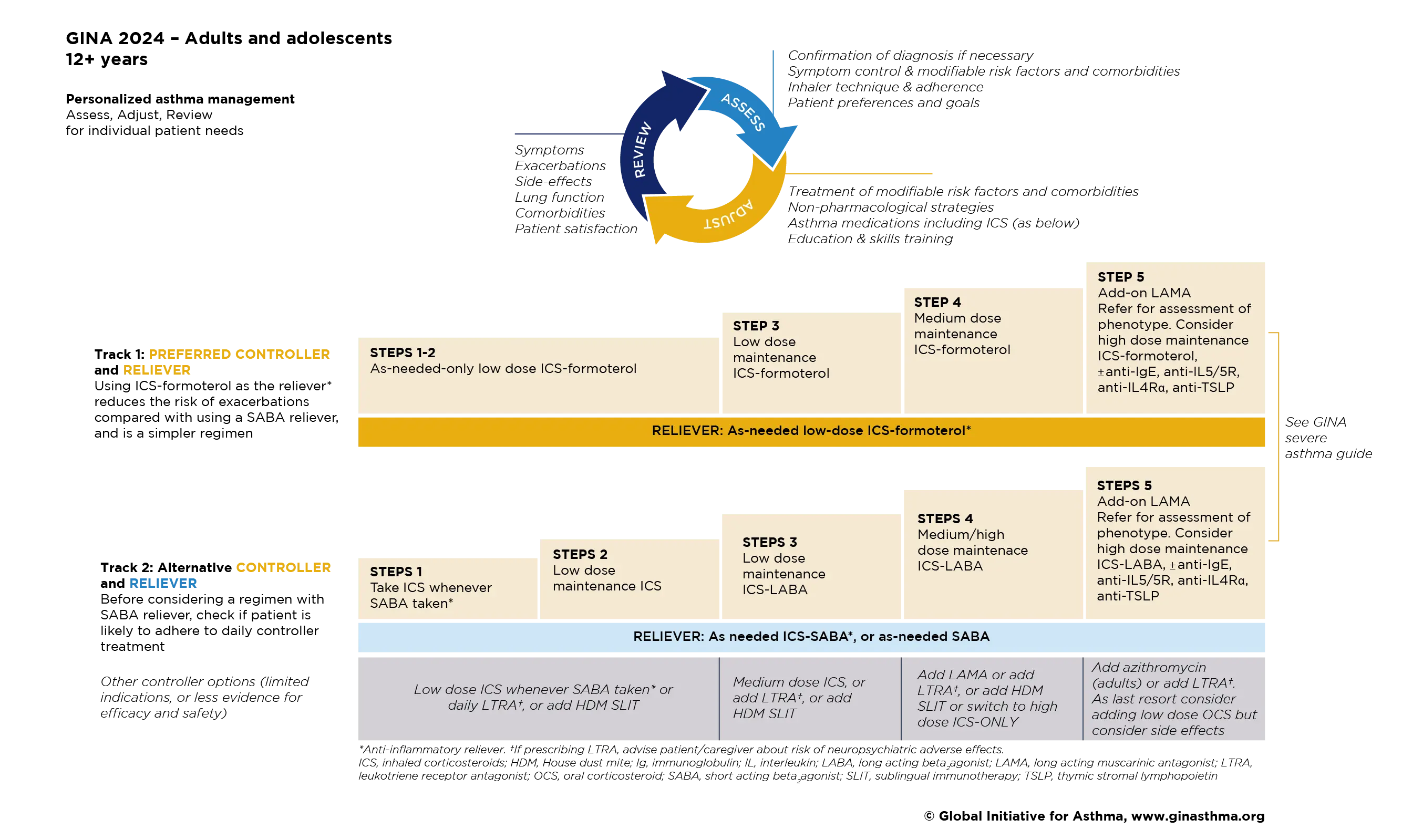
Asthma management1
The GINA goal of asthma management is to achieve the best possible long-term outcomes for the individual patient, including symptom control and minimizing risk of asthma-related mortality, exacerbations, persistent airflow limitation and treatment side effects.
Click here to download the 2024 GINA report to understand how to manage patients with asthma
Personalized management for adults and adolescents to control symptoms and minimize future risk.1
References
- Global strategy for Asthma Management and Prevention (2024 update). (Accessed August 1, 2024, at https://ginasthma.org/2024-report/)
- Silva GE, Sherrill DL, Guerra S, Barbee RA. Asthma as a risk factor for COPD in a longitudinal study. Chest. 2004 Jul;126(1):59-65.
- Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD Overlap Syndrome (ACOS): A Systematic Review and Meta Analysis. PLoS One. 2015;10(9):e0136065.
- Yawn BP. Differential assessment and management of asthma vs chronic obstructive pulmonary disease. Medscape J Med 2009;11:20.
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2024 report). (Accessed April 21, 2024, at https://goldcopd.org/wp-content/uploads/2024/02/GOLD-2024_v1.2-11Jan24_WMV.pdf.)
- Higham A, Beech A, Wolosianka S, Jackson N, Long G, Kolsum U, et al. Type 2 inflammation in eosinophilic chronic obstructive pulmonary disease. Allergy. 2021;76(6):1861-64.
- Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R; ECLIPSE investigators. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014;44(6):1697-700.
- Yun JH, Lamb A, Chase R, Singh D, Parker MM, Saferali A, et al; COPDGene and ECLIPSE Investigators. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(6):2037-2047.e10.
MAT-SA-2400418/V1/SEP24