- Article
- Source: Campus Sanofi
- May 23, 2025
A video series on round table discussions featuring experts: Biomarkers to guide COPD management

COPD is a heterogenous and progressive disease, driven by distinct chronic immune processes. In a round table discussion, leading respiratory experts discussed
- What are the current unmet needs for patients with COPD?
- How do different inflammatory pathways in COPD impact disease pathobiology and progression?
- Biomarkers to guide COPD management.
The round table was chaired by Professor Paola Rogliani of the University of Rome, Italy. Other respiratory experts on the panel were:
Dr. MeiLan Han, Professor of pulmonary critical care medicine at the University of Michigan, Ann Arbor, MI, USA.
Dr. Marc Miravitlles, a chest physician from the Hospital Universitari Vall d’Hebron, Barcelona, Spain.
Biomarkers to guide COPD management
Check out the video below to gain valuable insights on this topic from the respiratory experts
In this video, Dr. Miravitlles discusses the biomarkers to guide COPD management, followed by a panel discussion with other experts.
Risk factors for frequent exacerbation
Dr. Miravitlles started his talk by highlighting that patients with frequent exacerbations are the most challenging and also those having the worst prognosis. Therefore, one of the aims of therapy in COPD is to prevent exacerbations. He explained that to understand the frequent exacerbator phenotype, we need to know the characteristics of these patients. “It is not restricted to very severe patients,” he added.
Patients who have a history of frequent exacerbations are those likely to suffer frequent exacerbations in the future.
Other risk factors for frequent exacerbations include:1
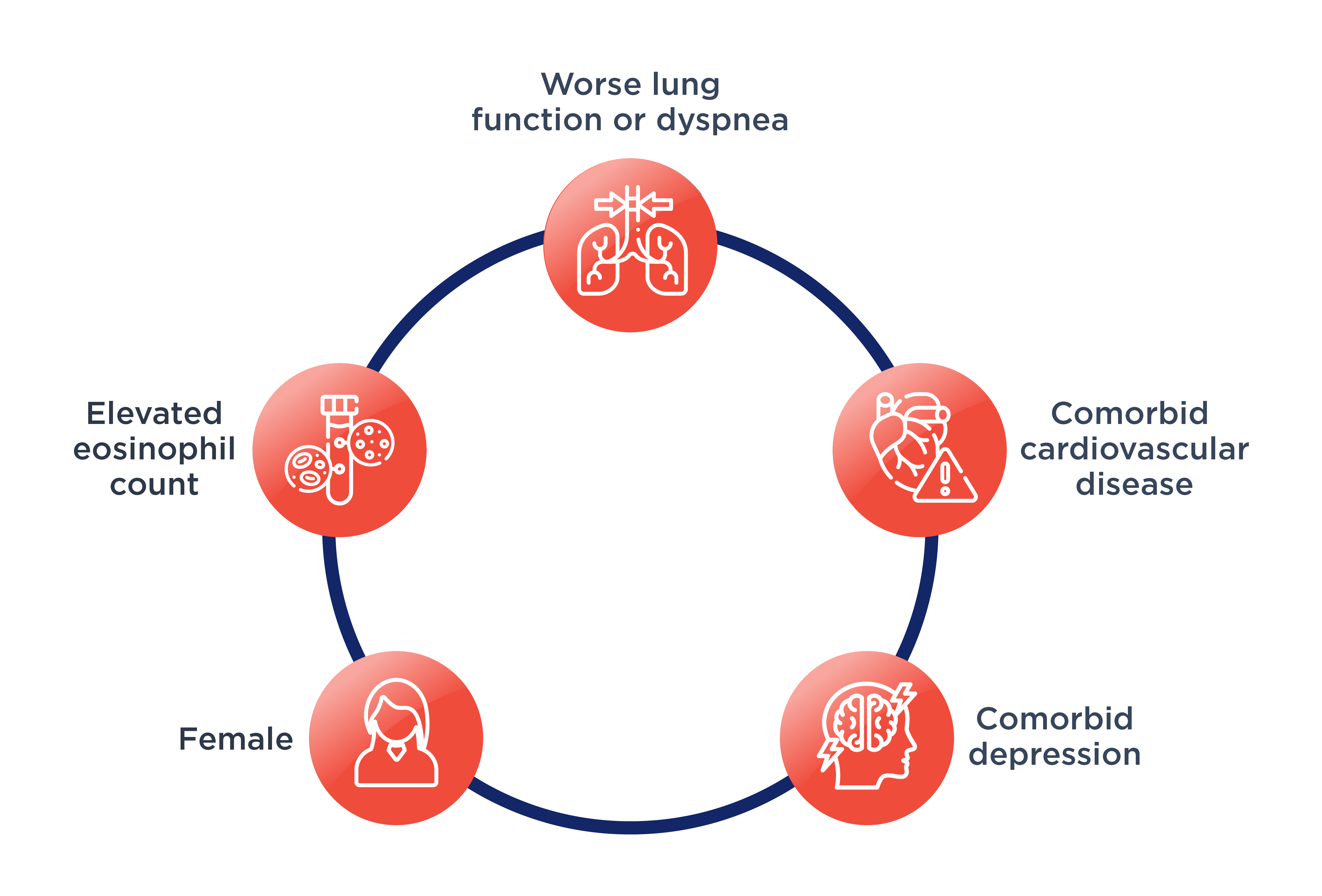
Dr. Miravitlles highlighted that the characteristics to identify the frequent exacerbator phenotype in COPD and those requiring more intensive treatment are patients who had more frequent exacerbations or severe exacerbations that resulted in hospital admission, in the past. Furthermore, patients with frequent exacerbations exhibit different mechanisms for exacerbations and are required to be treated differently.
Blood eosinophil count (EOS) as a biomarker in COPD: GOLD scientific committee findings
Dr. Miravitlles emphasized that there is a need for biomarkers in COPD to guide the practicing clinicians about the first choice of treatment for each type of exacerbation. He further added, “Blood eosinophils (EOS) are a good biomarker to identify COPD patients with a predominant type 2 inflammation.”
Read more about blood eosinophils as a biomarker in patients with COPD
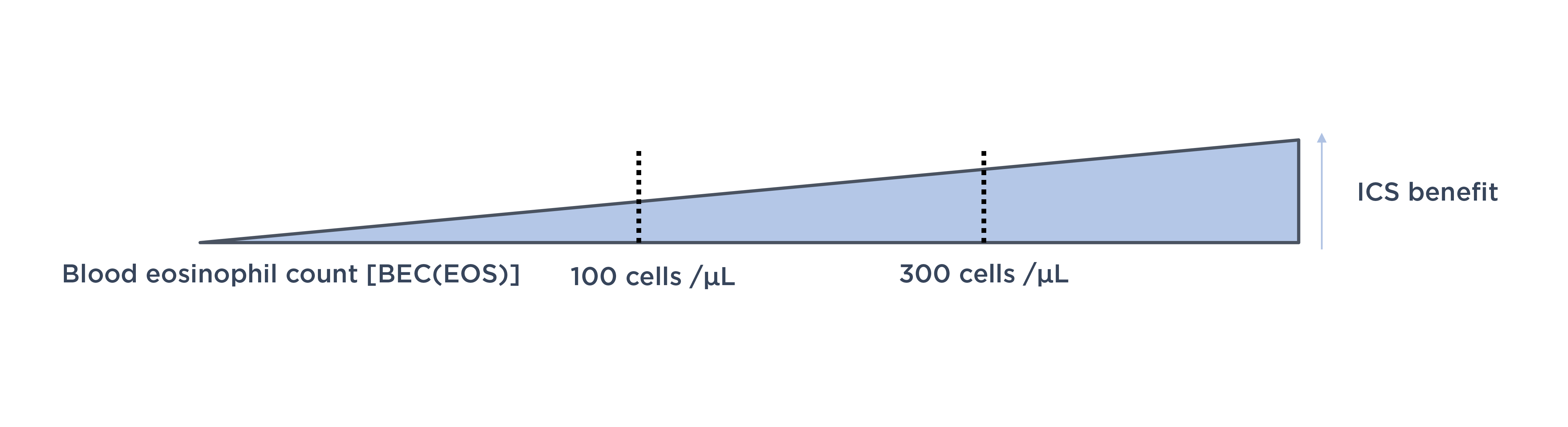
Prediction of benefits from inhaled corticosteroids (ICS)
Blood eosinophil count (BEC [EOS]) should be combined with exacerbation history to predict ICS effects.3 Dr. Miravitlles explained that there are several clinical trials which have demonstrated the use of BEC (EOS) to predict the effects of ICS in preventing exacerbations, particularly when combined with exacerbation history. However, relationship between BEC (EOS) and ICS effects is continuous,3 and there is no clear threshold for BEC (EOS). Thresholds of <100 cells/μL and ≥300 cells/μL help to identify individuals with the lowest and greatest, respectively, likelihood of ICS benefit.3
Dr. Miravitlles cautioned that if BEC (EOS) is <100 cells/µL, there is almost no effect of ICS and their long-term use can result in more side effects. “In contrast, patients with BEC (EOS) ≥300 cells/µL respond very well to ICS and have a significant reduction in the risk of exacerbations”, he added.
Type 2 inflammation
Dr. Miravitlles emphasized, “It is clear that there is some relationship between BEC (EOS) and markers of type 2 inflammation.” He further highlighted that the relationship is not perfect, but the relationship between BEC (EOS) and eosinophils in the lower airways is significant.
Learn more about type inflammation in COPD from decoding type 2 inflammation in COPD: An expert’s perspective
Future risk of exacerbations/disease progression
In younger individuals without COPD, higher BEC (EOS) are associated with increased risk of decline of forced expiratory volume in 1 second and development of COPD.3 “So, it is an important biomarker to identify these risks in a wider population”, Dr. Miravitlles pointed out.
BEC (EOS) cannot be used as a standalone biomarker of future risk without considering exacerbation risk and ICS use.3
Dr. Miravitlles summarized his discussion by saying, “We have an easy-to-use biomarker to identify a particular subgroup of patients who are more likely to respond to some types of drugs, such as ICS and this biomarker can be accessed at all levels of healthcare, even in primary care.”
Panel discussion
Dr. Miravitlles’s presentation was followed by individual perspectives of the panel of experts on biomarkers to guide COPD management.
Dr. Rogliani opened the panel discussion by highlighting the need for more biomarkers in the future to characterize patients with chronic obstructive diseases. She further added that BEC (EOS) is easy to use and easy to detect, but we will need a more precise way to detect it, which is still confined to research settings.
She concluded by saying, “BEC (EOS) is a useful biomarker, and it is helpful to manage patients in daily practice in our daily routine.”
Dr. Han emphasized that the cut offs for BEC (EOS) of 300 cells/µL for initial use of triple therapy and 100 cells/µL for escalating therapy in patients who are continuing to exacerbate on current therapy, provided in the GOLD document are sort of guideposts. She thought that the data for eosinophil-guided ICS, specifically for eosinophils <100 cells/µL was on the weaker side, whereas benefits appear stronger as the eosinophil levels go higher.
She stated, “In an ideal world we would be using sputum eosinophils, but that’s a challenging biomarker to get outside of our research setting.” “There is a potential for other biomarkers in the future,” she further pointed out.
Dr. Miravitlles added his thoughts, “BEC (EOS) is not a perfect biomarker, but is good enough to be used in clinical practice.” He further emphasized that with the evidence available at present, it is good enough in clinical practice for specialists and general practitioners.
References
- Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, Varghese P. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020 Mar;73:1-6. doi: 10.1016/j.ejim.2019.12.014. Epub 2020 Jan 16. PMID: 31954592.
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2025 report) (Accessed on May 13, 2025 at https://goldcopd.org/2025-gold-report/)
- Singh D, Agusti A, Martinez FJ, Papi A, Pavord ID, Wedzicha JA, Vogelmeier CF, Halpin DMG. Blood Eosinophils and Chronic Obstructive Pulmonary Disease: A Global Initiative for Chronic Obstructive Lung Disease Science Committee 2022 Review. Am J Respir Crit Care Med. 2022 Jul 1;206(1):17-24. doi: 10.1164/rccm.202201-0209PP. PMID: 35737975.
MAT-GLB-2400917