- Article
- Source: Campus Sanofi
- May 23, 2025
A video series on round table discussions featuring experts: Current unmet needs for patients with COPD

COPD is a heterogenous and progressive disease, driven by distinct chronic immune processes. In a round table discussion, leading respiratory experts discussed
- What are the current unmet needs for patients with COPD?
- How do different inflammatory pathways in COPD impact disease pathobiology and progression?
- Biomarkers to guide COPD management.
The round table was chaired by Professor Paola Rogliani of the University of Rome, Italy. Other respiratory experts on the panel were:
- Dr. MeiLan Han, Professor of Pulmonary Critical Care Medicine at the University of Michigan, Ann Arbor, MI, USA.
- Dr. Marc Miravitlles, a chest physician from the Hospital Universitari Vall d’Hebron, Barcelona, Spain.
What are the current unmet needs for patients with COPD?
Watch the video below to gain insights on this topic from the respiratory experts
In this video, Dr. Miravitlles discusses the current unmet needs in patients with COPD, followed by a panel discussion with other experts.
How Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines chronic obstructive pulmonary disease (COPD)?
COPD is a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, expectoration and/or exacerbations) due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.1
According to Dr. Miravitlles, “Despite airflow obstruction in all patients with COPD, they may have very different types of disease.”
Global burden of COPD
COPD is a leading cause of morbidity and mortality.2 Global burden of COPD continues to increase.2 COPD is currently the third leading cause of death worldwide and the seventh leading cause of poor health and disability.3
Smoking is the leading risk factor for the development of COPD.4,5 Dr. Miravitlles highlighted, “Cigarette smoking is the leading cause of COPD in most developed countries — in the United States, in Europe, Japan and around the world.” However, 25%–45% of people with COPD in the United States and other developed countries reportedly have never smoked.4 In low- and middle-income countries, up to 70% of cases of COPD are non-smokers.6
Second-hand smoke exposure has been implicated as a potential risk factor for the development of COPD in non-smokers.5 Non-smoking risk factors may include indoor4 and outdoor air pollution and infections.6
COPD exacerbations
Incidence and prevalence
Studies have shown that exacerbations are common among patients with COPD.7,8,9
Dr. Miravitlles noted, “More than one-half of patients with moderate-to-severe COPD experience exacerbations.”
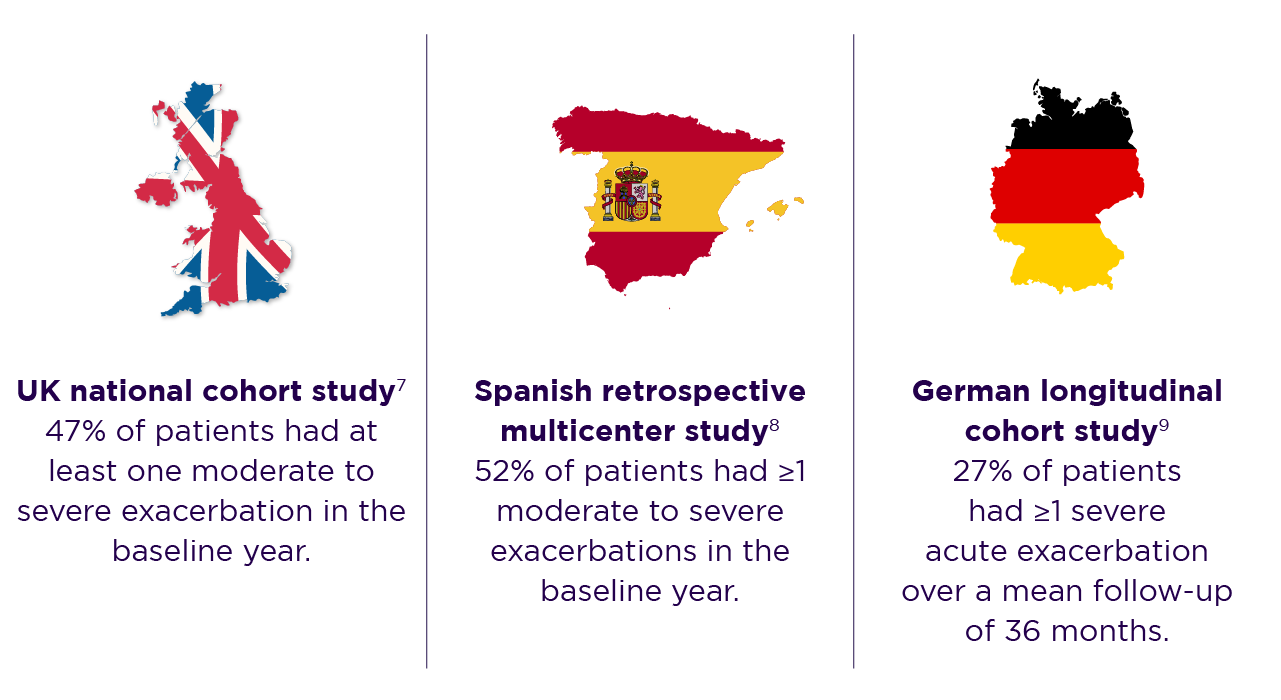
Of 52% of patients with moderate-to-severe exacerbations in the Spanish study, 12% had 1 severe exacerbation, 8% had ≥2 moderate and/or severe exacerbations, and 9% had ≥3 moderate-to-severe exacerbations.8
Clinical impact
Dr. Miravitlles highlighted the clinical impact of COPD exacerbations, “Patients with frequent exacerbations also have an accelerated decline in lung function.” Moreover, exacerbations can have potentially irreversible effects on lung function. In a retrospective analysis of the 4-year, randomized, double-blind, placebo-controlled, parallel group UPLIFT® (Understanding Potential Long-term Impacts on Function with Tiotropium) trial, the annual decline in post-bronchodilator FEV1 was nearly doubled after a single moderate-to-severe exacerbation.10
For more information, please watch the video on the burden and risk of exacerbations in COPD presented by Dr. Surya Bhatt, a distinguished professor of medicine at the University of Alabama at Birmingham and a COPD researcher.
An observational study conducted using data from the UK clinical practice research datalink (CPRD) Aurum database, reported that the frequency of future exacerbations increased with increased frequency and severity of exacerbations at baseline in patients with COPD.
As emphasized by Dr. Miravitlles, “Even a single moderate exacerbation increases risk of future exacerbation events,” the adjusted incidence rate ratio for future exacerbation (vs 0 exacerbation) was 1.70 (95% CI: 1.66–1.74) with 1 moderate exacerbation according to the CPRD Aurum database study.7
Read this article to find out more about the the impact of exacerbations in COPD.
The CPRD Aurum database study also reported an association between increased frequency and severity of baseline exacerbations with mortality (all cause/COPD-related/cardiovascular-related).7
Impact on quality of life
While explaining impact of exacerbations, Dr. Miravitlles further highlighted, “It’s not just lung function, patients with COPD complain of impairment in quality of life, which is even more impaired when they experience a severe exacerbation.” Exacerbations have an impact on daily activities of the patient, such as walking, sleeping, talking, and sexual life.11 Furthermore, reduced physical activity levels have been associated with an increased risk of further exacerbations and mortality.11
“There is a vicious circle of more symptoms, reduced activity, even more symptoms. We need to break this vicious circle by providing adequate treatment for not only acute exacerbations, but also for stable COPD”, Dr. Miravitlles pointed out.
COPD exacerbations despite maximal inhaled therapy
Dr. Miravitlles called attention to frequent exacerbations despite triple therapy with inhaled corticosteroids (ICS), long-acting muscarinic antagonist (LAMA) and long-acting β2 agonist (LABA), representing a crucial unmet need,12 “There are patients who despite optimal or maximal inhaled therapy are still experiencing exacerbations.”
Discover more about understanding and managing COPD exacerbations.
In this context, Dr. Miravitlles discussed a UK study involving 43,753 patients with COPD receiving maintenance therapy. Of the overall study population, 6480 (15%) patients were frequent exacerbators, defined as those who had experienced ≥1 severe or ≥2 moderate exacerbations despite ≥3 months of continuous treatment with triple therapy in the prior 12 months.12 During the 12-month follow-up in the UK study, frequent exacerbators reported a mean of 2.55 (vs 1.19) exacerbations even after triple therapy. These patients also had a significantly higher risk of COPD-related death (5.8% vs 2.1%, P <0.0001) than other maintenance therapy-treated patients. Importantly, almost one-quarter of frequent exacerbators exhibited a high blood eosinophil count (BEC [EOS]) (≥250 cells/µL) and ≥3 exacerbations.12
Learn more about blood eosinophils as a biomarker in patients with COPD.
Unmet needs in COPD
In his concluding slide, Dr. Miravitlles presented the conclusions and recommendations reached by the Lancet Commission from their analysis of the current landscape of COPD.2
COPD diagnosis relies almost exclusively on post-bronchodilator spirometry despite the heterogeneity of COPD. However, post-bronchodilator spirometry is neither sensitive for early pathological changes nor predictive of symptoms.2 As a result, COPD is often underdiagnosed or diagnosis is delayed, often until lung function is substantially impaired.2 Thus, making disease management more challenging.
The Lancet commission put forth urgent recommendations for driving transformational change and assessing progress, acknowledging that evidence to support their proposals is currently lacking.2
Dr. Miravitlles concluded, “so far, the guidelines recommend a kind of treatment that is quite simplistic in the sense that despite the heterogeneity of the disease, we do not have evidence to recommend a more personalized therapy. Therefore, we are still treating the majority of patients in a quite a standardized way. As a result, some patients, particularly moderate to severe, are still experiencing exacerbations despite the therapy.”
Panel discussion
Following Dr. Miravitlles presentation, the panel of experts added their views on the current unmet needs in patients with COPD.
Dr. Rogliani pointed out, “Post-bronchodilation spirometry is inadequate to detect early phase of the disease, which can really have an impact in terms of the natural history of the disease.” She further added that exacerbations are very different in terms of their nature, occurrence, and management approach.
Dr. Han opined, “Not all COPD is related to tobacco smoke.” She added that patients may get COPD from occupational exposures, recurrent respiratory infections, asthma along with early life factors; therefore, exposure history is important from public health perspective.
She emphasized upon, “Increasing public awareness, increasing physician awareness and trying to track and identify patients with a different idiotype and move them into clinical trials.”
On this note, Dr. Rogliani highlighted the need for a different approach towards COPD.
Dr. Miravitlles agreed and highlighted, “We need to address different aspects of the disease, starting with the risk factors.” He also added that there is a need to pay attention to the most severe patients, who are on the so-called maximum therapy.
Dr. Han said that good therapies are available, but the primary need is for better therapies, because patients suffering from frequent exacerbations and significant morbidity and disability, despite the currently available therapies, still there.
References
-
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2025 report) (Accessed on May 13, 2025 at https://goldcopd.org/2025-gold-report/)
-
Stolz D, Mkorombindo T, Schumann DM, Agusti A, Ash SY, Bafadhel M, et al. Towards the elimination of chronic obstructive pulmonary disease: a Lancet Commission. Lancet. 2022 Sep 17;400(10356):921-972. doi: 10.1016/S0140-6736(22)01273-9. Epub 2022 Sep 5. PMID: 36075255; PMCID: PMC11260396.
-
World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). Key facts. Available at: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). Last accessed: October 08, 2024.
-
Pando-Sandoval A, Ruano-Ravina A, Candal-Pedreira C, Rodríguez-García C, Represas-Represas C, Golpe R, et al. Risk factors for chronic obstructive pulmonary disease in never-smokers: A systematic review. Clin Respir J. 2022 Apr;16(4):261-275. doi: 10.1111/crj.13479. Epub 2022 Feb 10. PMID: 35142054; PMCID: PMC9060104.
-
Wheaton AG, Liu Y, Croft JB, VanFrank B, Croxton TL, Punturieri A, et al. Chronic Obstructive Pulmonary Disease and Smoking Status - United States, 2017. MMWR Morb Mortal Wkly Rep. 2019 Jun 21;68(24):533-538. doi: 10.15585/mmwr.mm6824a1. PMID: 31220055; PMCID: PMC6586372.
-
Agustí A, Celli BR, Criner GJ, Halpin D, Anzueto A, Barnes P, et al. Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary. Arch Bronconeumol. 2023 Apr;59(4):232-248. English, Spanish. doi: 10.1016/j.arbres.2023.02.009. Epub 2023 Mar 1. PMID: 36933949.
-
Whittaker H, Rubino A, Müllerová H, Morris T, Varghese P, Xu Y, et al. Frequency and Severity of Exacerbations of COPD Associated with Future Risk of Exacerbations and Mortality: A UK Routine Health Care Data Study. Int J Chron Obstruct Pulmon Dis. 2022 Mar 3;17:427-437. doi: 10.2147/COPD.S346591. PMID: 35264849; PMCID: PMC8901192.
-
Soler-Cataluña JJ, Izquierdo JL, Juárez Campo M, Sicras-Mainar A, Nuevo J. Impact of COPD Exacerbations and Burden of Disease in Spain: AVOIDEX Study. Int J Chron Obstruct Pulmon Dis. 2023 Jun 8;18:1103-1114. doi: 10.2147/COPD.S406007. PMID: 37313500; PMCID: PMC10259458.
-
Vogelmeier CF, Rhodes K, Garbe E, Abram M, Halbach M, Müllerová H, et al. Elucidating the risk of cardiopulmonary consequences of an exacerbation of COPD: results of the EXACOS-CV study in Germany. BMJ Open Respir Res. 2024 Mar 30;11(1):e002153. doi: 10.1136/bmjresp-2023-002153. PMID: 38555102; PMCID: PMC10982767.
-
Halpin DMG, Decramer M, Celli BR, Mueller A, Metzdorf N, Tashkin DP. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017 Jul;128:85-91. doi: 10.1016/j.rmed.2017.04.013. Epub 2017 Apr 24. PMID: 28610675.
-
Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020 Mar;73:1-6. doi: 10.1016/j.ejim.2019.12.014. Epub 2020 Jan 16. PMID: 31954592.
-
Chen S, Miravitlles M, Rhee CK, Pavord ID, Jones R, Carter V, et al. Patients with Chronic Obstructive Pulmonary Disease and Evidence of Eosinophilic Inflammation Experience Exacerbations Despite Receiving Maximal Inhaled Maintenance Therapy. Int J Chron Obstruct Pulmon Dis. 2022 Sep 9;17:2187-2200. doi: 10.2147/COPD.S378649. PMID: 36110306; PMCID: PMC9470244.
MAT-GLB-2400917