- Article
- Source: Campus Sanofi
- May 23, 2025
Navigating the Hidden Burden: The Critical Role of Moderate Exacerbations in COPD

Recognizing Moderate Exacerbations: The Need for Vigilance
Moderate exacerbations are those that require treatment with short acting bronchodilators, systemic corticosteroids and/or antibiotics.2 Early recognition and prompt management of moderate exacerbations are critical to mitigating their impact on COPD progression and patient outcomes.
Criteria for moderate exacerbation2,4
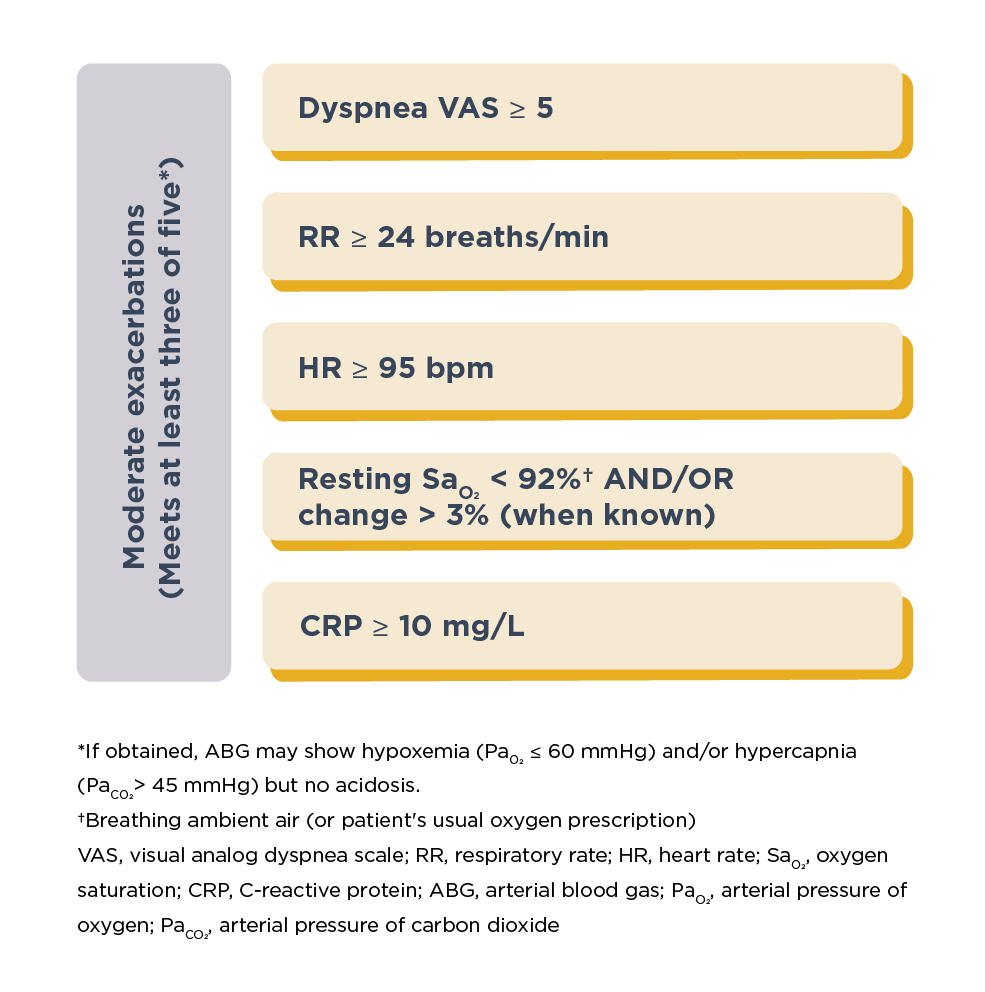
According to GOLD Group ABE assessment tool, patients with a history of 0 or 1 moderate exacerbation, not leading to hospitalization, but with significant symptom burden [CAT (COPD assessment test) ≥10 or a mMRC (modified Medical Research Council dyspnea questionnaire) ≥2] are categorized as GOLD Group B.2,5 Patients with ≥2 moderate exacerbations (or ≥1 exacerbation requiring hospitalization) are categorized as GOLD Group E, irrespective of symptom burden.2
For more information, please read GOLD recommendations for treatment and management of COPD.
Clinicians must be vigilant for key indicators that may signal a need for hospitalization:
Potential indicators for hospitalization assessment*2
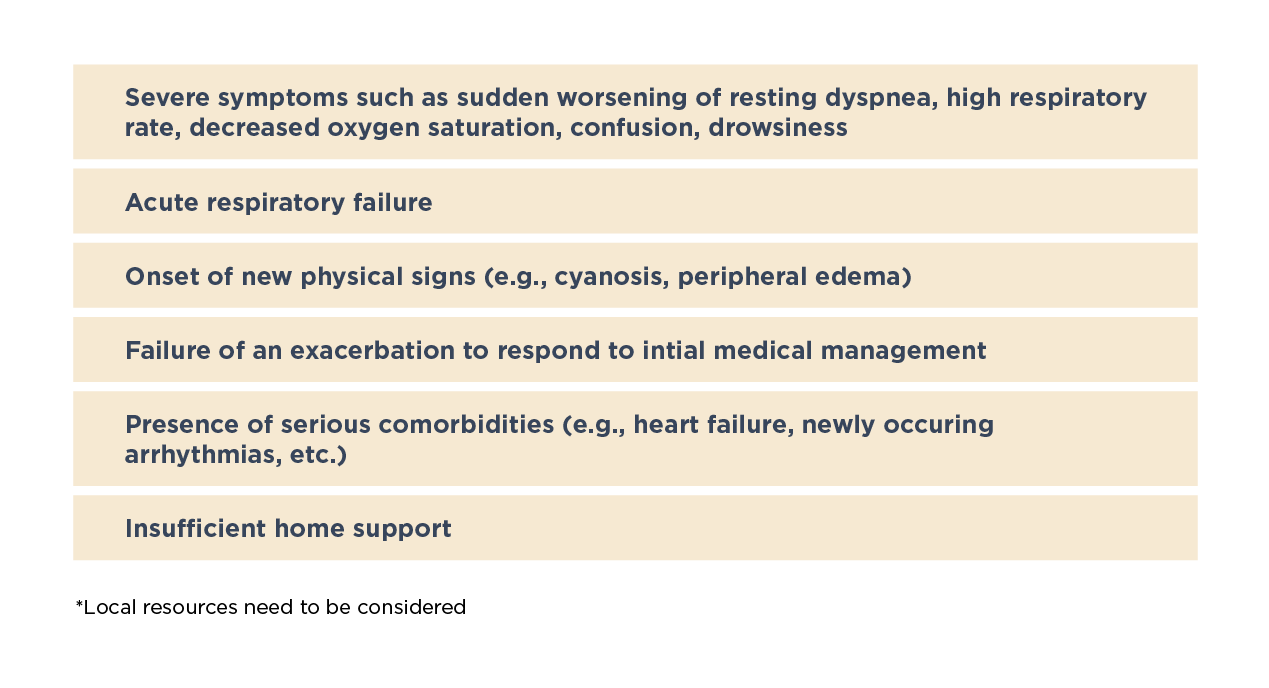
Recognizing these clinical signs and intervening promptly can help prevent moderate exacerbations from escalating to more severe levels; thereby, reducing the overall burden of COPD. Remote home monitoring of patients, including the use of patient-reported outcomes and spirometry,6 is essential to detecting exacerbations early and improving overall management.
Please click on the link to know what tests can help diagnose and monitor your patients with COPD?
Moderate Exacerbation: The Unseen Drivers of COPD Progression
Moderate and/or severe exacerbations are not merely transient events; they are pivotal in shaping the trajectory of COPD.5 Acute moderate exacerbations are linked with worsening of airflow obstruction and lung hyperinflation.7 Furthermore, patients with frequent moderate to severe exacerbations exhibit a more rapid decline in lung function — forced expiratory volume in 1 second of 40 mL/year and peak expiratory flow of 2.9 L/min/year — compared with those with infrequent exacerbations.8
Dr Surya Bhatt, a distinguished professor of medicine at the University of Alabama at Birmingham and a COPD researcher talks about the burden and risk of exacerbations in COPD.
The likelihood of subsequent moderate and severe exacerbations, and death are increased by 1.58 times, 2.08 times and 1.85 times, respectively, for 3 years following one moderate exacerbation with high symptom burden compared with no exacerbation.5 The risk of future exacerbations increases with even one episode of moderate exacerbation; thus, each episode is critical.5
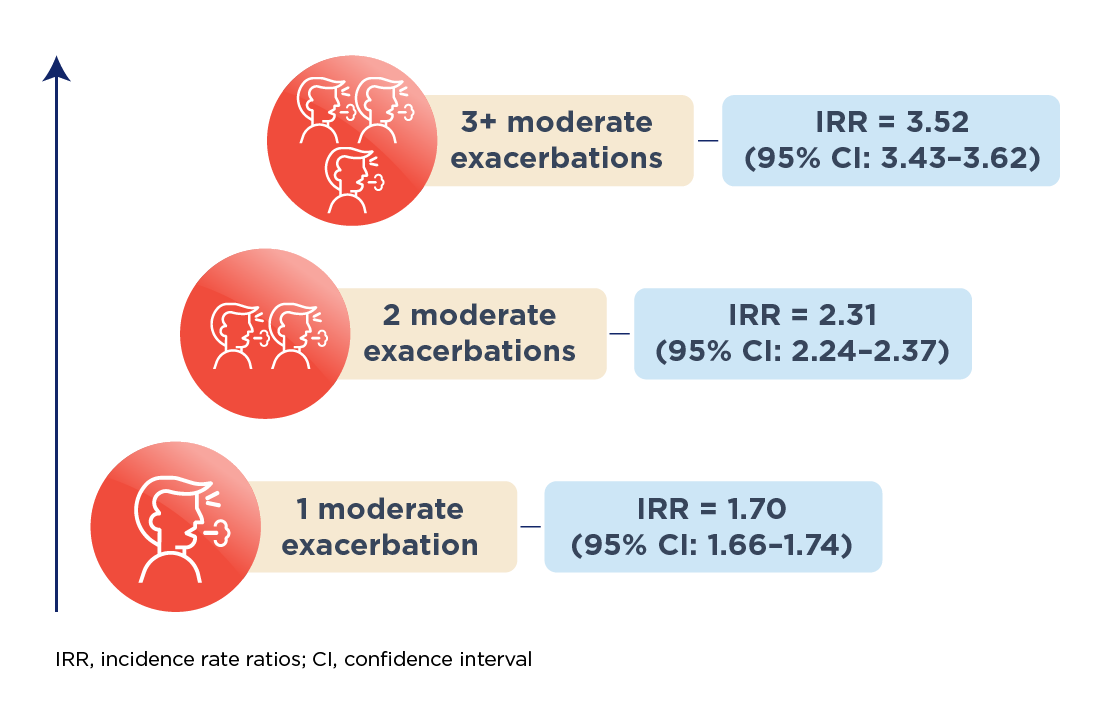
Risk of future exacerbations with increasing frequency of moderate exacerbations9
For healthcare providers (HCP), the ability to recognize and treat frequent exacerbations early is crucial. This requires a proactive approach to COPD management, including increased HCP awareness on treatment recommendations, patient education, the development of integrated care action plans, and the provision of timely access to appropriate therapies.10 Such strategies are essential to maintaining disease control, preventing exacerbations from escalating, and reducing the overall burden of COPD on both patients and the healthcare system.
Learn more about understanding and managing COPD exacerbations.
The Ripple Effect: Impact of Moderate Exacerbations on Quality of Life (QoL)
Frequent exacerbations significantly impact the QoL for patients with COPD.11,12 The psychological impact of exacerbations is also considerable. Studies have shown that patients with frequent exacerbations are more likely to suffer from anxiety, post-traumatic stress and depression,13 with reportedly high prevalence (depression: 19.4%–50.0%; anxiety 9.3%–58.0%) soon after recovery.14 This psychological burden not only affects QoL, but also complicates disease management by impairing treatment adherence and increasing the risk of future exacerbations.15
Read this article to learn more about the impact of exacerbations in COPD.
Economically, moderate exacerbations can contribute to substantial healthcare costs. Data indicate that the direct costs associated with moderate exacerbation can range from $248 to $1,011 per episode, depending on the setting of care.16 Indirect costs, including lost productivity and the need for informal caregiving, further amplify the economic impact.17 Overall, exacerbations account for approximately 50%–75% of the total annual COPD-related healthcare costs, highlighting their significant economic burden.16
In conclusion, moderate exacerbations play a critical role in the clinical course of COPD, with significant implications for both patient outcomes and healthcare resources. By prioritizing the early recognition and management of these exacerbations, healthcare providers can help mitigate their impact on disease progression and improve the overall QoL for patients with COPD.18 This approach, supported by appropriate maintenance treatment and patient-centered care such as pulmonary rehabilitation, is essential to achieving optimal outcomes in COPD management.10
References
- Wedzicha JA, Mackay AJ, Singh R. COPD exacerbations: impact and prevention. Breathe. 2013 Dec 1;9(6):434-40.doi: 10.1183/20734735.002913
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2025 report) (Accessed May 5, 2025, at https://goldcopd.org/2025-gold-report/).
- Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007 Sep 1;370(9589):786-96. doi: 10.1016/S0140-6736(07)61382-8. PMID: 17765528; PMCID: PMC7134993.
- Celli BR, Fabbri LM, Aaron SD, Agusti A, Brook R, Criner GJ, Franssen FME, Humbert M, Hurst JR, O'Donnell D, Pantoni L, Papi A, Rodriguez-Roisin R, Sethi S, Torres A, Vogelmeier CF, Wedzicha JA. An Updated Definition and Severity Classification of Chronic Obstructive Pulmonary Disease Exacerbations: The Rome Proposal. Am J Respir Crit Care Med. 2021 Dec 1;204(11):1251-1258. doi: 10.1164/rccm.202108-1819PP. PMID: 34570991.
- Løkke A, Hilberg O, Lange P, Ibsen R, Stratelis G, de Fine Licht S, Lykkegaard J. Disease Trajectories and Impact of One Moderate Exacerbation in Gold B COPD Patients. Int J Chron Obstruct Pulmon Dis. 2022 Mar 16;17:569-578. doi: 10.2147/COPD.S344669. PMID: 35321533; PMCID: PMC8937604.
- Johns DP, Walters JA, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thorac Dis. 2014 Nov;6(11):1557-69. doi: 10.3978/j.issn.2072-1439.2014.08.18. PMID: 25478197; PMCID: PMC4255165.
- Parker CM, Voduc N, Aaron SD, Webb KA, O'Donnell DE. Physiological changes during symptom recovery from moderate exacerbations of COPD. Eur Respir J. 2005 Sep;26(3):420-8. doi: 10.1183/09031936.05.00136304. PMID: 16135722.
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002 Oct;57(10):847-52. doi: 10.1136/thorax.57.10.847. Erratum in: Thorax. 2008 Aug;63(8):753. PMID: 12324669; PMCID: PMC1746193.
- Whittaker H, Rubino A, Müllerová H, Morris T, Varghese P, Xu Y, De Nigris E, Quint JK. Frequency and Severity of Exacerbations of COPD Associated with Future Risk of Exacerbations and Mortality: A UK Routine Health Care Data Study. Int J Chron Obstruct Pulmon Dis. 2022 Mar 3;17:427-437. doi: 10.2147/COPD.S346591. PMID: 35264849; PMCID: PMC8901192.
- Bollmeier SG, Hartmann AP. Management of chronic obstructive pulmonary disease: A review focusing on exacerbations. Am J Health Syst Pharm. 2020 Feb 7;77(4):259-268. doi: 10.1093/ajhp/zxz306. PMID: 31930287; PMCID: PMC7005599.
- Guo J, Chen Y, Zhang W, Tong S, Dong J. Moderate and severe exacerbations have a significant impact on health-related quality of life, utility, and lung function in patients with chronic obstructive pulmonary disease: A meta-analysis. Int J Surg. 2020 Jun;78:28-35. doi: 10.1016/j.ijsu.2020.04.010. Epub 2020 Apr 15. PMID: 32304896.
- Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F, Verea H, Murio C, Ros F, Vidal R; IMPAC Study Group. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax. 2004 May;59(5):387-95. doi: 10.1136/thx.2003.008730. PMID: 15115864; PMCID: PMC1746989.
- Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, Varghese P. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020 Mar;73:1-6. doi: 10.1016/j.ejim.2019.12.014. Epub 2020 Jan 16. PMID: 31954592.
- Maurer J, Rebbapragada V, Borson S, Goldstein R, Kunik ME, Yohannes AM, Hanania NA; ACCP Workshop Panel on Anxiety and Depression in COPD. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008 Oct;134(4 Suppl):43S-56S. doi: 10.1378/chest.08-0342. PMID: 18842932; PMCID: PMC2849676.
- Wang J, Willis K, Barson E, Smallwood N. The complexity of mental health care for people with COPD: a qualitative study of clinicians' perspectives. NPJ Prim Care Respir Med. 2021 Jul 22;31(1):40. doi: 10.1038/s41533-021-00252-w. PMID: 34294727; PMCID: PMC8298614.
- Toy EL, Gallagher KF, Stanley EL, Swensen AR, Duh MS. The economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a review. COPD. 2010 Jun;7(3):214-28. doi: 10.3109/15412555.2010.481697. PMID: 20486821.
- Patel JG, Nagar SP, Dalal AA. Indirect costs in chronic obstructive pulmonary disease: a review of the economic burden on employers and individuals in the United States. Int J Chron Obstruct Pulmon Dis. 2014 Mar 19;9:289-300. doi: 10.2147/COPD.S57157. PMID: 24672234; PMCID: PMC3964024.
- Yawn BP. Early identification of exacerbations in patients with chronic obstructive pulmonary disease. J Prim Care Community Health. 2013 Jan;4(1):75-80. doi: 10.1177/2150131912443827. Epub 2012 Apr 18. PMID: 23799693.
MAT-GLB-2400917