- Article
- Source: Campus Sanofi
- Jul 8, 2025
Understanding and Managing COPD Exacerbations

COPD exacerbation is an event characterized by increased dyspnea and/or cough and sputum that worsens in less than 14 days and may be accompanied with tachypnea and/or tachycardia.2
COPD exacerbations are often associated with increased local and systemic inflammation caused by airway infection, air pollutants, or other airway insults.2 Type 2 inflammation, characterized by raised eosinophil count, is associated with increased risk of COPD exacerbations.3
Click here to understand how type 2 inflammation is linked to the risk of COPD exacerbations.
The treatment goals of COPD exacerbations are to minimize the negative impact of the current exacerbation and to prevent occurrence of subsequent events.2 The risk of subsequent events has been shown to increase with each exacerbation.1 Furthermore, frequent COPD exacerbations lead to accelerated lung function decline4 and worsening of symptoms.2
To know more, listen to the podcast on COPD exacerbations and their impact on patients’ quality of life by Prof. Nicola Hanania, Professor of Medicine, Section Chief of Pulmonary Critical Care and Sleep Medicine at the Ben Taub Hospital in Houston, Texas, and Director of the Airways Clinical Research Center, ACRC at the Bear College of Medicine.
Pathophysiology of acute COPD exacerbation
COPD exacerbations are often associated with increased local and systemic inflammation.2 Air pollutants, such as particulate matter, sulfur dioxide, and cigarette smoke can increase exacerbations. 5,6
In stable COPD, there is an increase in the release of inflammatory cells such as T- lymphocytes and macrophages in the bronchial mucosa.6 In patients with stable, but more severe COPD, there is an increase in airway neutrophils, which further elevate during exacerbations.6
A substantial percentage of patients with COPD show raised eosinophils in the airways, lungs, and blood;2 however, significant variations in blood eosinophil levels are observed during both stable COPD and acute exacerbations.7 Eosinophilic inflammation has been attributed as a cause for exacerbations. Patients with raised eosinophils during stable disease experience frequent and severe exacerbations.7 Patients with mild COPD and exacerbations have also demonstrated an increased number of eosinophils in their airways on bronchial biopsy.6
To know more, please read the article Blood Eosinophils as a Biomarker in Patients with COPD.
According to Dr Surya Bhatt, a distinguished professor of medicine at the University of Alabama at Birmingham and a COPD researcher, the burden and risk of exacerbations in COPD is profound and "there's plenty of data to suggest that these exacerbations are associated with lung function decline."
Click here to watch the full video by Dr Surya Bhatt.
Etiology of acute COPD exacerbation
COPD exacerbations are triggered by a variety of factors including airway infection, air pollution or other airway insults, with viral infections being a key trigger.2
Viral infections result in more severe exacerbations that are associated with longer recovery times, compared with those triggered by other factors.2 Such exacerbations also have a greater likelihood of hospital admission. Human rhinovirus, influenza and parainfluenza and metapneumovirus are the most common viruses implicated in airway infections causing exacerbations and can be isolated within a week of onset of exacerbation.2
The exact role of bacteria as a causative agent in COPD exacerbations remains uncertain as the same bacteria were identified in both stable disease and during exacerbations.6 Short-term exposure to environmental pollutants, such as particulate matter and nitrous oxide, has been linked to increased exacerbations, hospital admissions, emergency room, and outpatient visits and increased mortality.2
Read more about the impact of exacerbations in COPD here.
Dr. Surya Bhatt highlights, "The hazard of mortality is about twice if you get two severe exacerbations as opposed to one severe exacerbation. And the hazard of mortality is fivefold if you get ten exacerbations as opposed to one severe exacerbation."
Click here to watch Dr. Surya Bhatt’s video where he talks about the burden and risk of exacerbations in COPD.
Symptoms of acute COPD exacerbation
COPD exacerbations may be associated with a wide range of clinical signs and symptoms.5 The signs and symptoms during exacerbation are similar to what the patients usually experience; however, their severity is increased. COPD exacerbations are associated with deterioration in airflow limitation and dynamic hyperinflation, occurring as a result of bronchospasm, airway edema and excessive sputum production due to airway inflammatory responses.6 These changes primarily contribute to increased dyspnea, the most common symptom experienced during exacerbations.6
The other symptoms of COPD exacerbation include severe and strenuous cough, increased sputum volume, change in sputum color from whitish to yellow/green, and hemoptysis.5 On physical examination, increase in expiratory wheezing and rhonchi may be evident along with warning signs of impending respiratory failure, such as paradoxical breathing and respiratory alternans due to muscle fatigue.5
COPD exacerbation criteria and diagnosis
Several staging systems for classification of the severity of COPD exacerbations without respiratory failure were used previously; however, none were prospectively validated.5 The 2025 GOLD report proposed a classification system for exacerbation severity, using the Delphi approach after an exhaustive literature review.2
Exacerbations can be classified as mild, moderate, and severe after their onset.2 Classification of COPD exacerbation severity should be followed up with identification of cause by viral testing, sputum culture or other investigations.
Classification of COPD exacerbation severity2,8
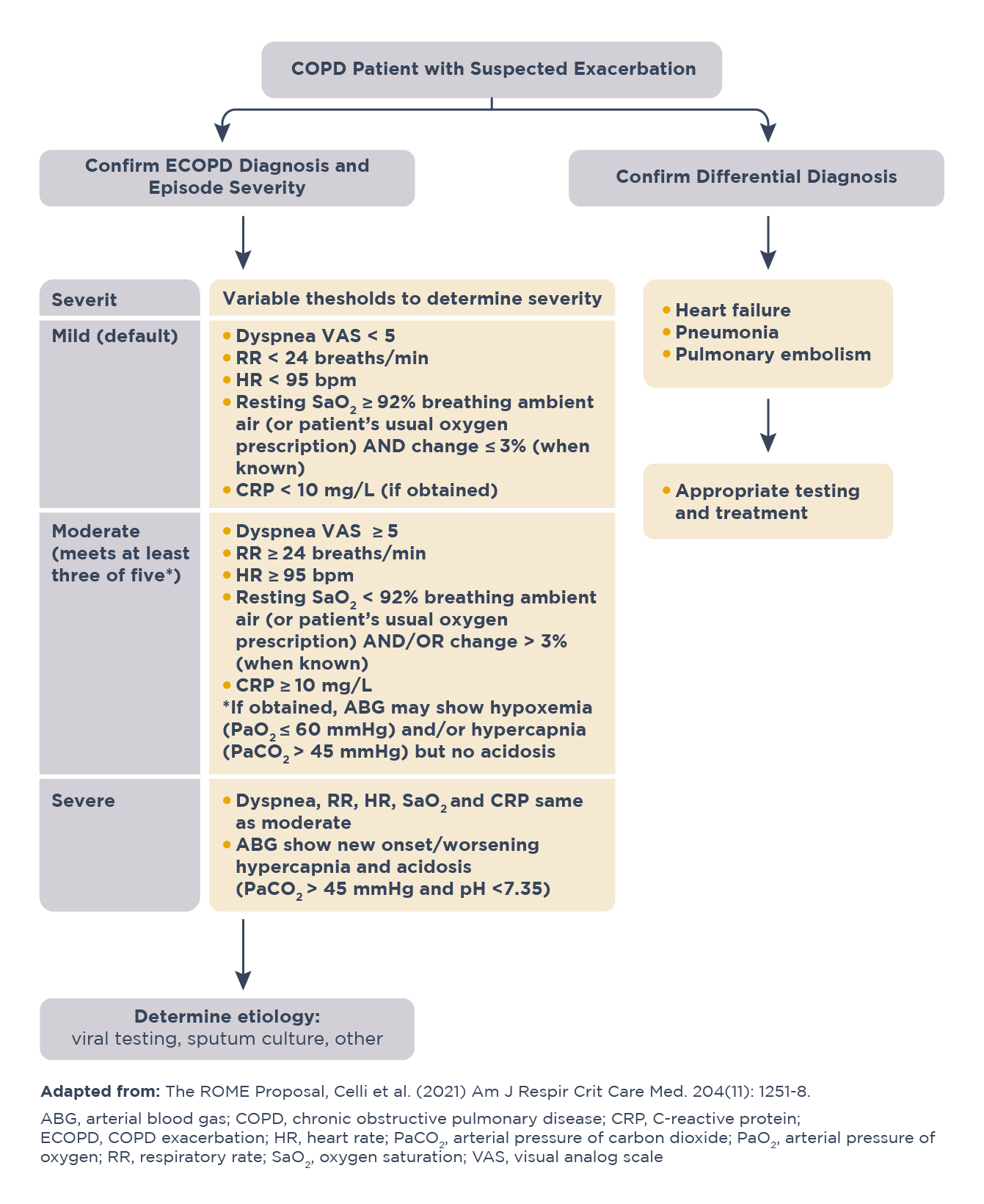
Click here for the 2025 GOLD report to learn more about COPD exacerbation diagnosis and severity.
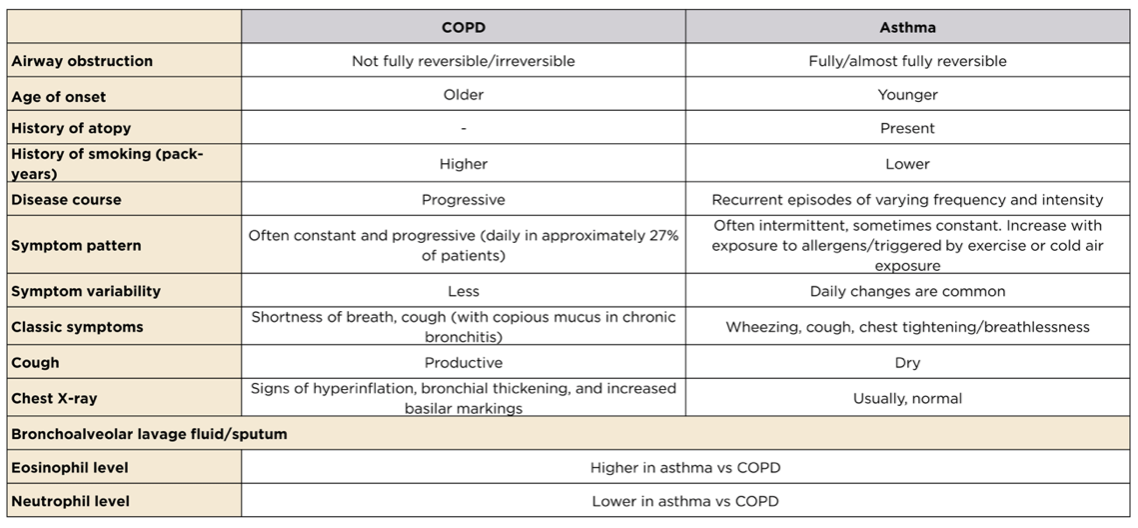
Differentiating asthma and COPD exacerbations9
Both asthma and COPD are obstructive lung disorders characterized by reduced pulmonary airflow due to increased inflammation and may present with acute exacerbations. Although the two conditions show some overlap in clinical features, the guideline-recommended management strategies and goals are different for both. Thus, it is important to distinguish between them for accurate diagnosis.
COPD and Asthma: Distinguishing features9
Treatment for acute COPD exacerbation
Minimizing the negative impact of ongoing COPD exacerbations and reducing the number and COPD exacerbation severity is critical to COPD management.10
Approximately four in five exacerbations are managed in outpatient setting using bronchodilators, corticosteroids and antibiotics.2 On arrival in emergency department, it should be assessed if the episode is life threatening and/or requires noninvasive ventilation.2
A life-threatening episode presents with signs of acute respiratory failure (respiratory rate, >24 breaths/minute; use of accessory respiratory muscles; acute changes in mental status; hypoxemia not improving with supplemental oxygen and requirement of FiO2 >40%; hypercarbia).2 Such patients should be admitted in a setting where they can be properly monitored and managed.2
Management of severe, but not life-threatening exacerbations2
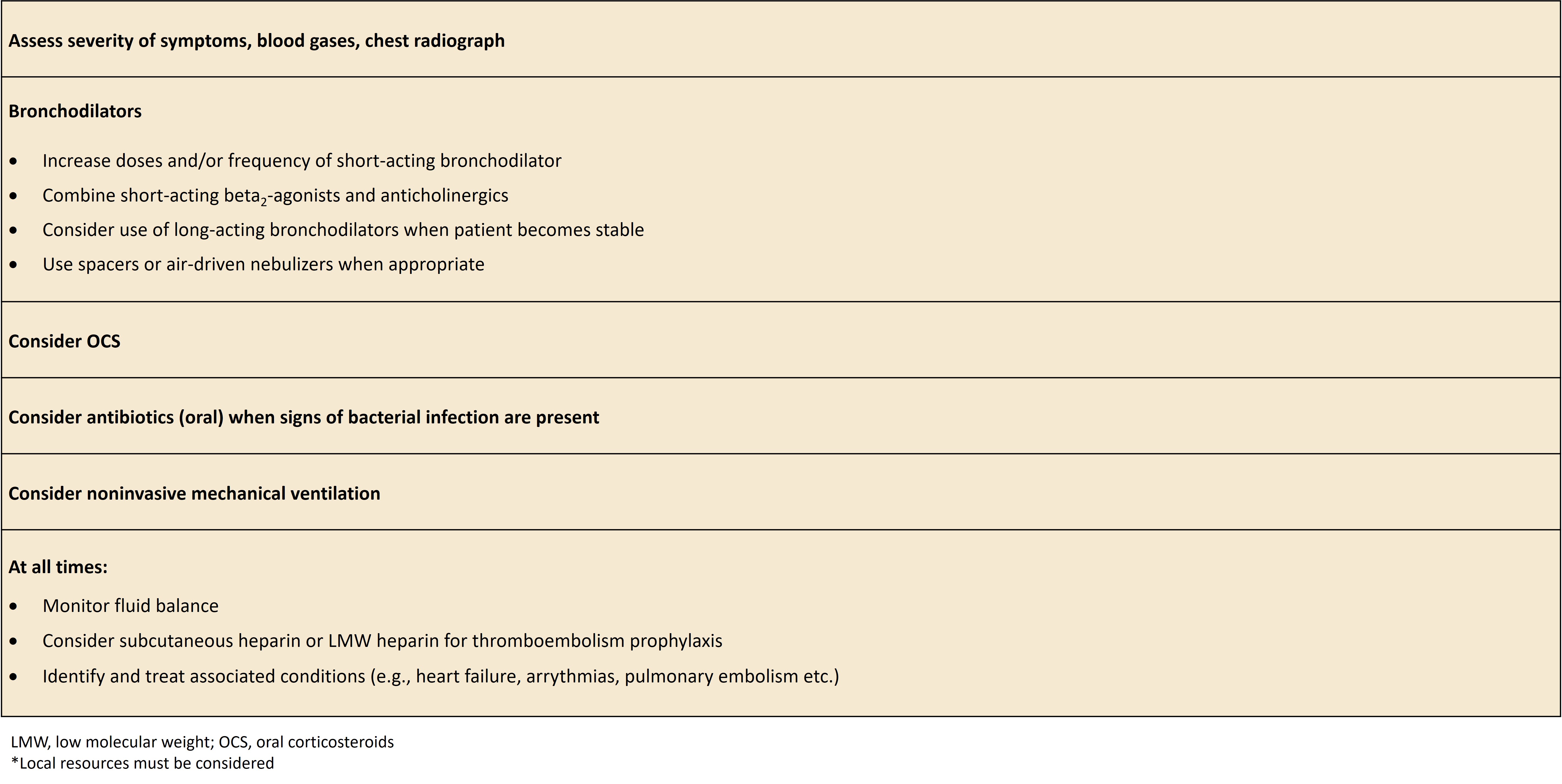
Learn more about the GOLD recommendations for treatment and management of COPD.
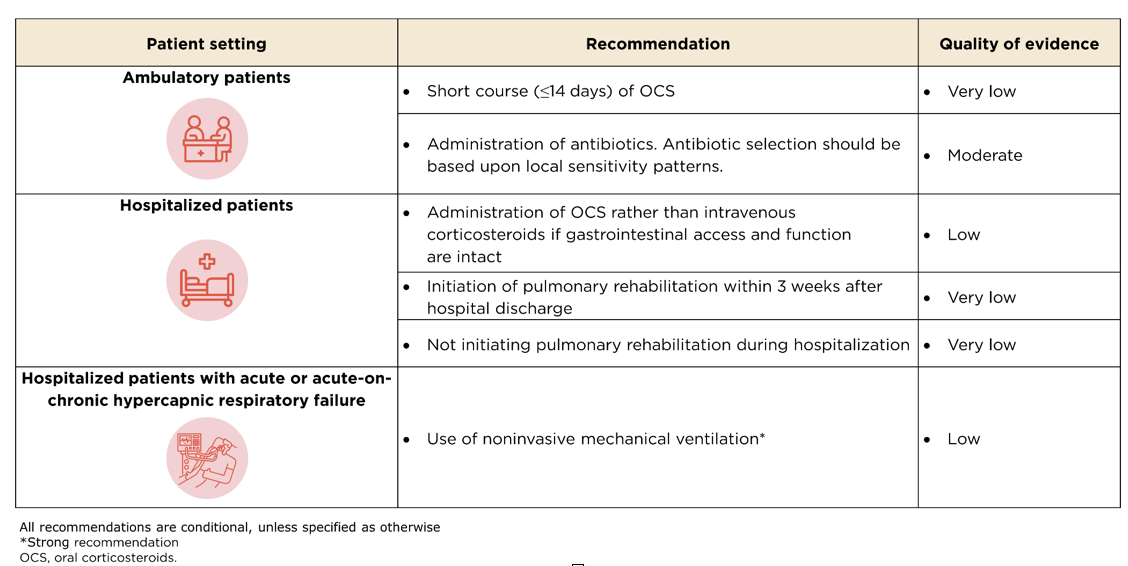
COPD exacerbation guidelines for treatment
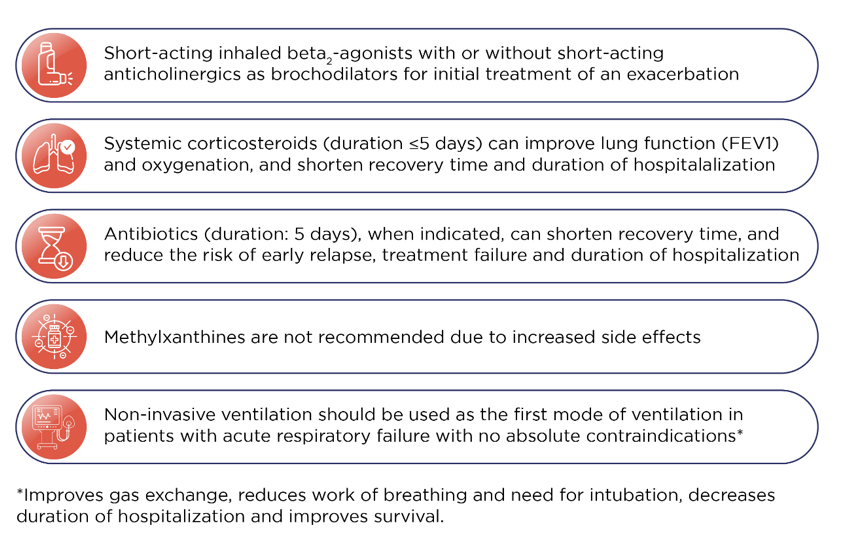
Please find below key recommendations by the European Respiratory Society (ERS) and American Thoracic Society (ATS) for the management of COPD exacerbations.
Key ERS/ATS recommendations for COPD exacerbation12
The GOLD 2025 report presents few key points for management of all COPD exacerbations.2
Key points for management of all COPD exacerbations2
References
- Suissa S, Dell’Anniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957-963.
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2025 report). (Accessed May 22, 2025, at https://goldcopd.org/2025-gold-report/.)
- Garudadri S, Woodruff PG. Targeting Chronic Obstructive Pulmonary Disease Phenotypes, Endotypes, and Biomarkers. Ann Am Thorac Soc. 2018 Dec;15(Suppl 4):S234-8.
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002 Oct;57(10):847-52.
- Maclntyre N, Huang YC. Acute exacerbations and respiratory failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc 2008;5:530-5.
- Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet 2007;370:786-96.
- David B, Bafadhel M, Koenderman L, De Soyza A. Eosinophilic inflammation in COPD: from an inflammatory marker to a treatable trait. Thorax 2021;76:188-95.
- Celli BR, Fabbri LM, Aaron SD, et al. An Updated Definition and Severity Classification of Chronic Obstructive Pulmonary Disease Exacerbations: The Rome Proposal. Am J Respir Crit Care Med. 2021 Dec 1;204(11):1251-58.
- Yawn BP. Differential assessment and management of asthma vs chronic obstructive pulmonary disease. Medscape J Med 2009;11:20.
- Vogelmeier CF, Roman-Rodriguez M, Singh D, Han MK, Rodriguez-Roisin R, Ferguson GT. Goals of COPD treatment: Focus on symptoms and exacerbations. Respir Med 2020;166:105938.
- Bhatt SP, Rabe KF, Hanania NA, et al. Dupilumab for COPD with Blood Eosinophil Evidence of Type 2 Inflammation. N Engl J Med. 2024;390(24):2274-2283.
- Wedzicha JAEC-C, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J 2017;49. (Accessed July 26, 2024, at https://publications.ersnet.org/content/erj/49/3/1600791)
MAT-GLB-2400917