- Article
- Source: Campus Sanofi
- Aug 4, 2025
Mechanism of Disease
In ITP, immune dysregulation lowers platelet counts through multiple pathways. Autoreactive B cells produce autoantibodies that target platelets for destruction by macrophages and impair megakaryocyte maturation, reducing platelet production. Autoantibodies may also destroy platelets through other mechanisms.
Immune system activity can also lead to elevated levels of inflammatory markers.1-6
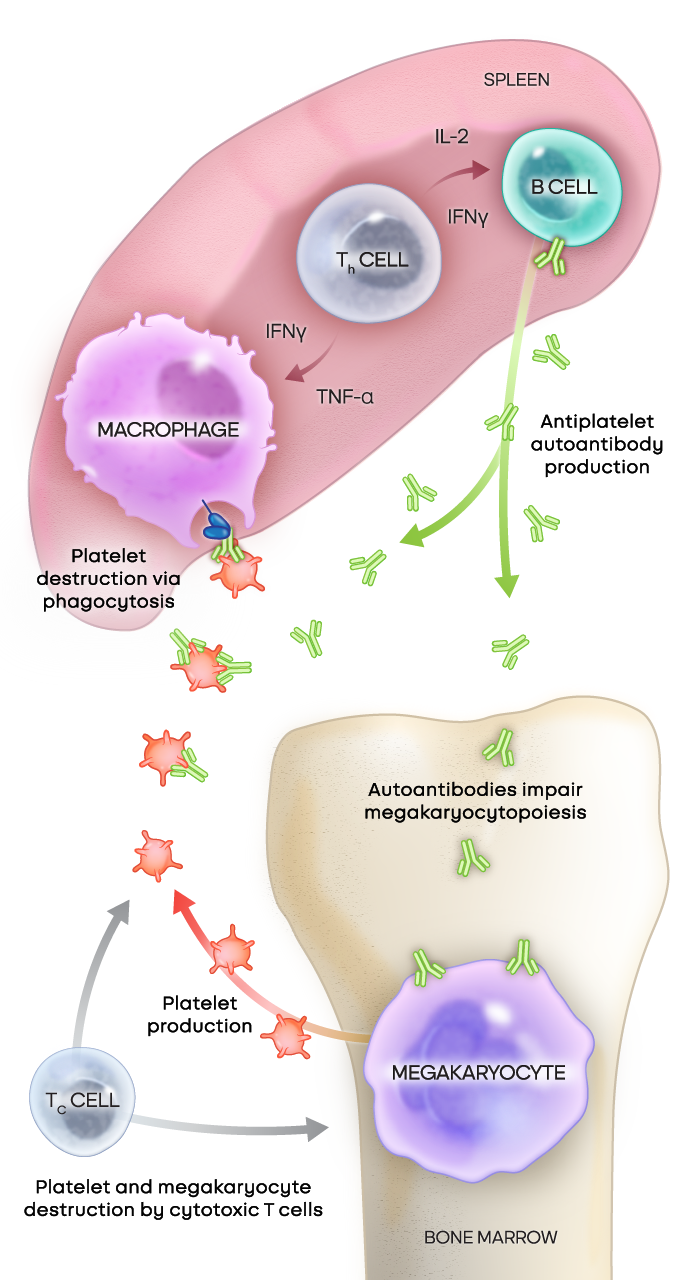
Adapted from Kashiwagi H, et al. Int J Hematol. 2013;98(1):24-33. © Japanese Society of Hematology (JSH).1
Treatments designed to achieve multi-immune modulation aim to better address the multiple dimension of ITP7,8
Watch the mechanism of disease (MOD) video to learn more about the multiple dimensions of ITP
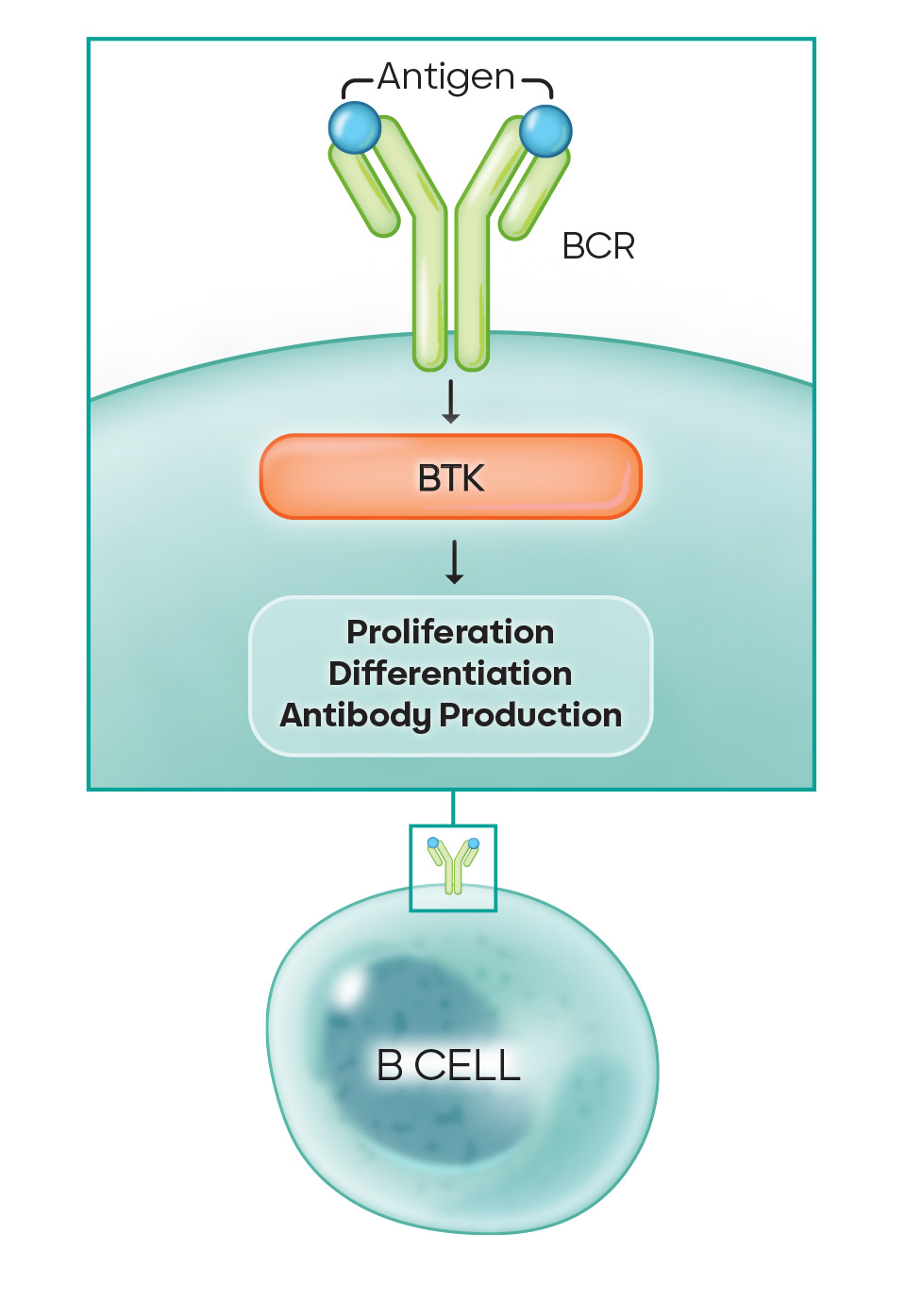
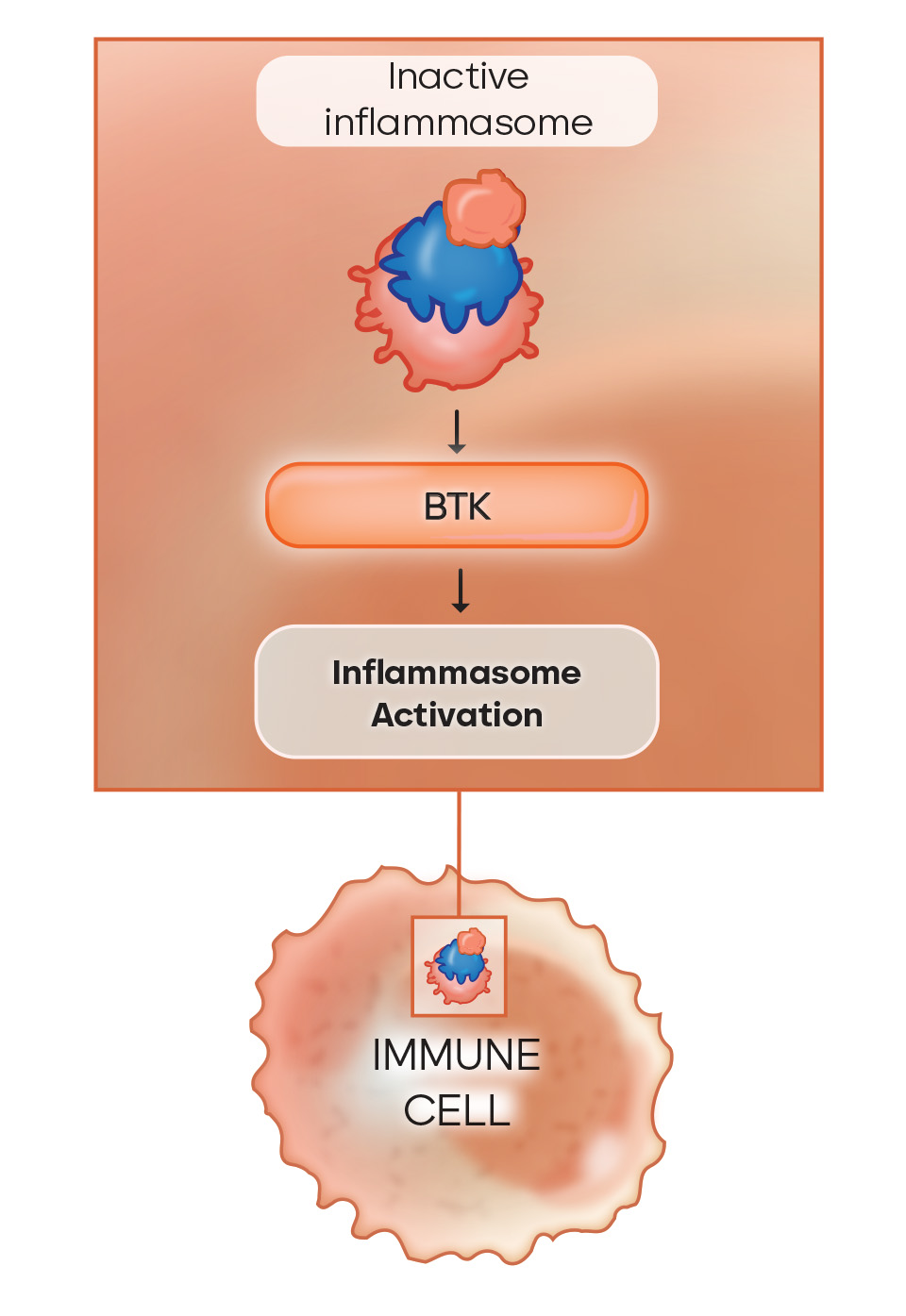
Bruton’s tyrosine kinase (BTK) plays a pivotal role in complex immune dysregulation9,10
B cells are responsible for the production of autoantibodies; macrophages are essential for phagocytosis; and the NLRP3 inflammasome plays a key role in systemic inflammation. All of these processes are regulated by BTK.9,10
- In B cells: The BTK pathway is crucial for proliferation, differentiation, and autoantibody production
- In macrophages: Various signalling pathways dependent on BTK drive phagocytosis, degranulation, and the production of inflammatory cytokines
- Systemically: BTK drives the production of mediators of inflammation like NLRP3 inflammasome, which can contribute to platelet destruction and systemic inflammation
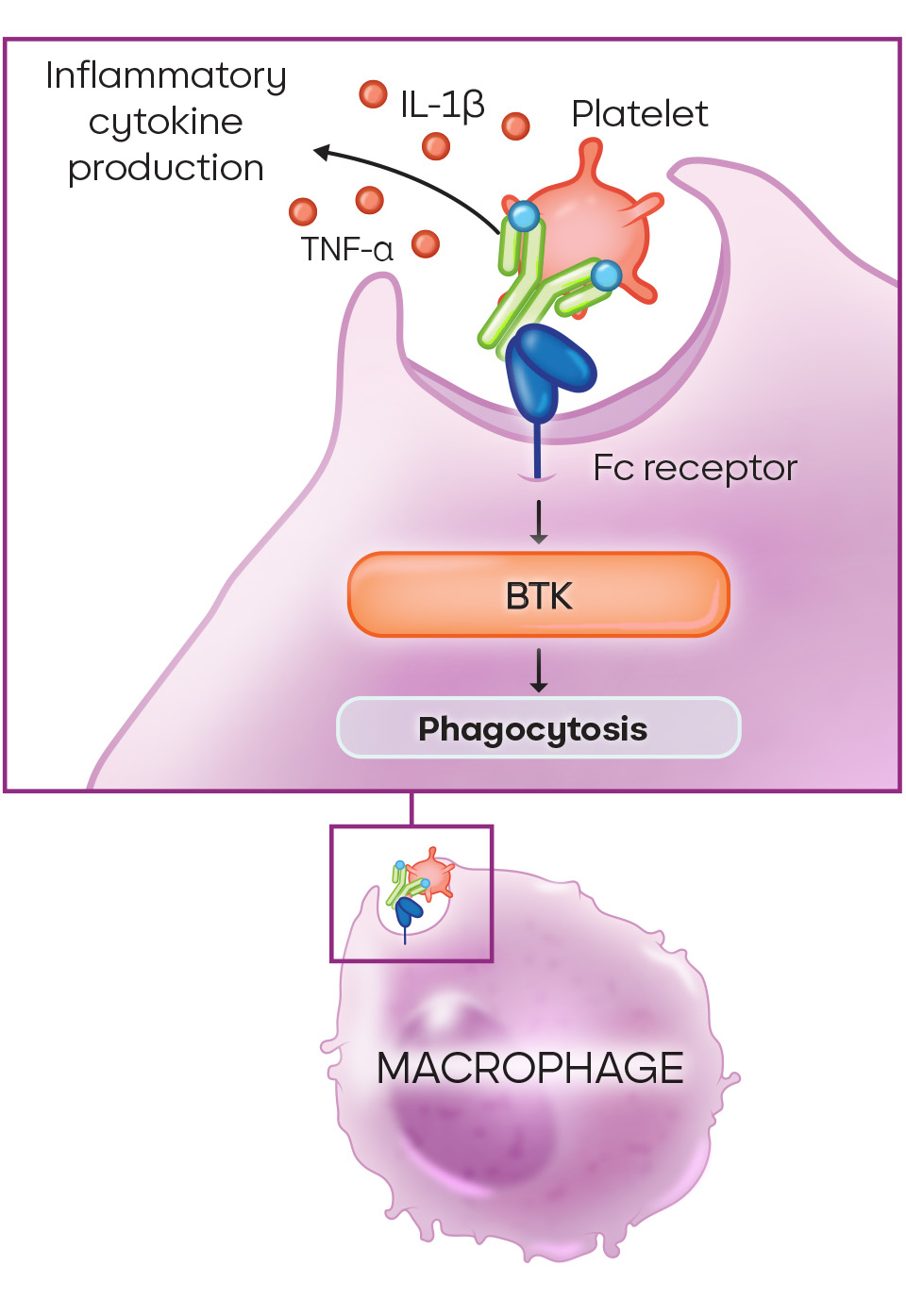
Patients living with ITP have elevated inflammatory markers, including10:
- TNF-α and IFN-γ
- IL-2 and IL-6
- NLRP3 inflammasome cytokines IL-1β and IL-18
BTK is implicated in the production or activation of these inflammatory markers and is a critical driver of inflammation.10
Other signalling pathways involved in the pathogenesis of ITP8
With incremental understanding of molecular mechanisms driving ITP pathology, it is becoming increasingly clear that multiple signalling pathways are involved in the pathogenesis and manifestation of the disease.8
ITP is about more than platelets
BCR, B-cell receptor; Fc, fragment crystallisable; IFN, interferon; IL, interleukin; NLRP3, nucleotide-binding domain, leucine-rich repeat and pyrin domain-containing protein 3; TNF, tumour necrosis factor.
Causes and pathophysiology of ITP1-4,8,11,12
ITP has an estimated prevalence of up to 9.5 per 100,000 people. The causes and pathophysiology of immune thrombocytopenia (ITP), historically called idiopathic thrombocytopenic purpura or immune thrombocytopenic purpura, are multifactorial and trigger a wide range of symptoms.
The pathophysiology of ITP is complex, involving various immune cells and different organs. Platelet destruction and inhibition of thrombopoiesis (platelet production) are key drivers of the disease. Current treatments for ITP aim to target these mechanisms of immune thrombocytopenia.
Our understanding of the pathophysiology of ITP is expanding and opening up new treatment possibilities for more targeted therapies and overall disease control.
What are the causes of ITP12-14
The cause of ITP in adults can be differentiated by whether the disease is primary or secondary ITP.
In primary ITP, the underlying causes remain unidentified—this is why it was previously known as idiopathic thrombocytopenic purpura. This is the most common cause of ITP, with approximately 80% of ITP patients diagnosed with primary ITP.
In contrast, secondary ITP is caused by known factors such as certain medications, infections, or cancers.
It is often associated with persistent autoimmunity and underlying autoimmune diseases including systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS).
Chronic ITP is characterised by the persistence of symptoms for more than 12 months after the initial diagnosis. Chronic ITP is more common in adults than in children. Recent studies suggest genetic factors, including polymorphisms in cytokine receptor genes and genes regulating T cell activity, may influence the susceptibility for chronic ITP. However, more research is needed to fully understand the causes of chronic ITP.
References
1. Kashiwagi H, Tomiyama Y. Pathophysiology and management of primary immune thrombocytopenia. Int J Hematol. 2013;98(1):24-33. 2. Andreescu M. The link between immune thrombocytopenia and the cytokine profile: a bridge to new therapeutical targets. Front Hematol. 2023;2:1191178. 3. Qiao J, Liu Y, Li X, et al. Elevated expression of NLRP3 in patients with immune thrombocytopenia. Immunol Res. 2016;64(2):431-437. 4. Schifferli A, Cavalli F, Godeau B, et al. Understanding immune thrombocytopenia: looking out of the box. Front Med (Lausanne). 2021;8:613192. 5. Wang S, Liu Y, Li G, Feng Q, Hou M, Peng J. Reduced intracellular antioxidant capacity in platelets contributes to primary immune thrombocytopenia via ROS-NLRP3-caspase-1 pathway. Thromb Res. 2021;199:1-9. 6. Nelson VS, Jolink AC, Amini SN, et al. Platelets in ITP: victims in charge of their own fate? Cells. 2021;10(11):3235. 7. Audia S, Bonnotte B. Emerging therapies in immune thrombocytopenia. J Clin Med. 2021;10(5):1004. 8. Mingot-Castellano ME, Bastida JM, Caballero-Navarro G, et al. Novel therapies to address unmet needs in ITP. Pharmaceuticals (Basel). 2022;15(7):779. 9. Zhu S, Gokhale S, Jung J, et al. Multifaceted immunomodulatory effects of the BTK inhibitors ibrutinib and acalabrutinib on different immune cell subsets – beyond B lymphocytes. Front Cell Dev Biol. 2021;9:727531. 10. Neys SFH, Hendriks RW, Corneth OBJ. Targeting Bruton’s tyrosine kinase in inflammatory and autoimmune pathologies. Front Cell Dev Biol. 2021;9:668131. 11. Lambert MP, Gernsheimer TB. Clinical updates in adult immune thrombocytopenia. Blood. 2017;129(21):2829-2835. 12. Matzdorff A, Meyer O, Ostermann H, et al. Immune thrombocytopenia – current diagnostics and therapy: recommendations of a joint working group of DGHO, ӦGHO, SGH, GPOH, and DGTI. Oncol Res Treat. 2018;41(suppl 5):1-30. 13. Pietras NM, Gupta N, Justiz Vaillant AA, Pearson-Shaver AL. Immune Thrombocytopenia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 5, 2024. 14. Georgi JA, Middeke JM, Bornhäuser M, Matzdorff A, Trautmann-Grill K. Deciphering the genetic basis of immune thrombocytopenia: current evidence for genetic predisposition in adult ITP. Blood Adv. 2023;7(14):3710-3724.
MAT-GLB-2500852-v1.0-06/2025