- Article
- Source: Campus Sanofi
- Aug 6, 2025
Living with ITP

In a study, patients living with ITP rated their health-related quality of life (HRQoL) significantly worse than the general US population. They also reported worse HRQoL than patients living with hypertension, arthritis, or cancer, and similar to that of patients living with diabetes.1*
*The study used the Short-Form 36 questionnaire to evaluate the HRQoL of 73 adult ITP patients compared with that of the general US population and of patients with 6 other relatively common chronic disorders.1
ITP can impact patient HRQoL in multiple ways, including:

Fatigue
Reported as severe by patients with ITP, often regardless of platelet counts2
Heavy menstrual bleeding
Rated by patients and doctors as one of the most severe ITP symptoms2

Thromboembolic events (TEs)
Compared to patients without ITP, there is up to a 2x higher risk of TEs3
Cerebral microbleeds (CMBs)
Associated with lower platelet count and longer disease duration4
Fatigue is common and can be severe in patients with ITP2
In the Immune Thrombocytopenia World Impact Survey (I-WISh)* of 1507 patients and 472 physicians, patients rated functional, psychological, and emotional aspects of their condition. In I-WISh2:

58% of patients reported fatigue at diagnosis (n=870/1507),2

and 73% of those patients rated fatigue as severe (n=637/870)2
Even in patients with low disease activity, prevalence of severe fatigue exists, and fatigue persists even after platelet counts have increased. Disease activity alone does not explain variance in ITP.2,5
Factors that may play a role in fatigue5,6:
- Inflammation
- Physical and functional well-being
- Physical activity
Research shows that ITP is also linked to reduced activity and a notable increase in general, mental, and physical fatigue.7,8
The exact causes of fatigue and the underlying pathophysiology are not fully understood. However, ITP-related excessive and prolonged bleeding leads to iron deficiency and anaemia, which can be contributors to fatigue. Learn more about the causes and pathophysiology of ITP.6,9,10
Furthermore, ITP-related activity restrictions can result in frustration, social withdrawal, and mood decline.7,11
I actually avoid everything in my everyday life that drains a lot of energy.
*I-WISh was an online, cross-sectional survey of patients with ITP and haematologists or haemato-oncologists who treat patients with ITP in 13 countries. The patient questionnaire collected information on demographics and diagnosis, symptoms of ITP, HRQoL and emotion associated with ITP, impact of ITP on work, finances, and support, treatment received, and patient and physician relationship. The physician survey comprised 6 sections that collected information on demographics, diagnosis of ITP and patient caseload, symptoms of ITP, impact of ITP on aspects of patients’ physical, emotional, HRQoL, social health, treatment patterns, and patient and physician relationship. There were 2 questions about the emotional impact of ITP, and the responses were based on a 7-point Likert scale (1 = never, 7 = a great deal). There was 1 additional question on the need for professional support.7
Heavy menstrual bleeding can have a major negative impact on patient HRQoL2

45% of women with ITP reported heavy menstrual bleeding at diagnosis2
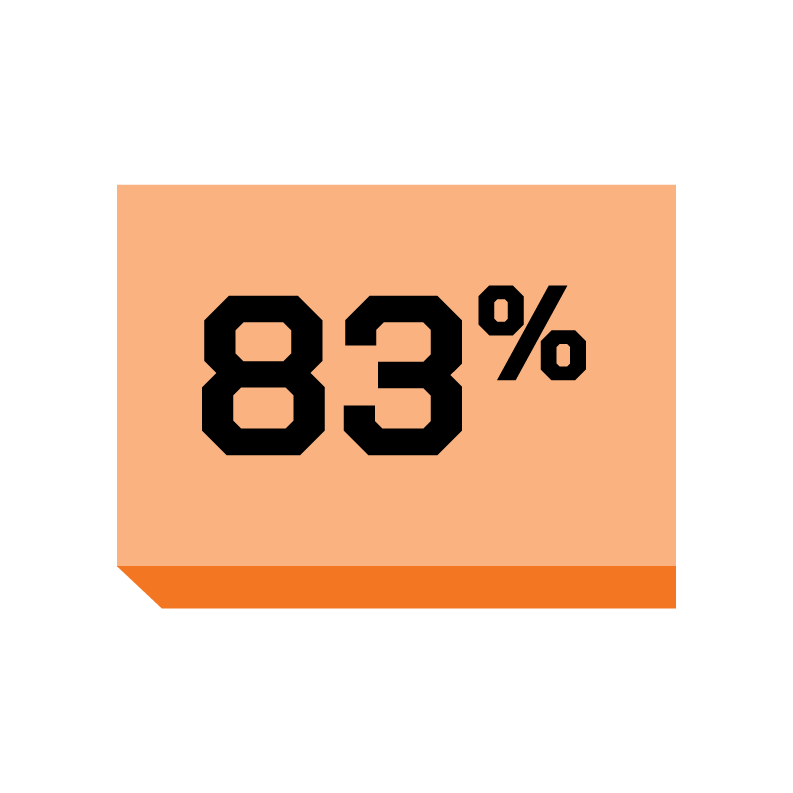
and 83% of those said it was one of their most severe symptoms2
Thromboembolic events (TEs) are also more common among patients with ITP3
Patients with ITP face up to a 2X higher risk of TEs compared to patients without ITP3*
Risk factors for TEs in ITP12:
- Mechanisms of ITP itself
- Patient comorbidities and past history
- Current ITP treatments patient may be taking
*Adjusted risk ratio of 1.7 in a retrospective cohort study of 1140 patients with ITP and 5657 patients without ITP.3
Patients with ITP might also suffer from cerebral microbleeds4

In a 2020 study published in Blood,* 43% of patients with ITP had CMBs (n=21/49)4
CMBs were associated with lower platelet count and longer disease duration. The strong association between CMBs and ITP duration could indicate that CMBs may accumulate over time.4
*A cross-sectional prospective study of 49 patients with ITP and nadir platelet counts <30,000/μL and 18 age-matched healthy controls that used susceptibility-weighted magnetic resonance imaging (MRI) to detect CMBs as a marker of occult haemorrhage.4
Neurological symptoms and cognitive effects of immune thrombocytopenia
50% of patients with ITP experience some level of cognitive impairment (N=69)13
Neurological manifestations in ITP without clinically significant bleeding are rare.14
However, patients with ITP might also suffer from cognitive impairment.14
Can ITP cause headaches?
Individuals with ITP can suffer from headaches and migraines. A sudden headache in ITP patients can also be an indication of the rare but severe complication of intracranial haemorrhage (ICH), which can cause other neurological symptoms.2,15-17
References
1. McMillan R, Bussel JB, George JN, Lalla D, Nichol JL. Self-reported health-related quality of life in adults with chronic immune thrombocytopenic purpura. Am J Hematol. 2008;83(2):150-154. 2. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (iWISh): patient and physician perceptions of diagnosis, signs and symptoms, and treatment. Am J Hematol. 2021;96(2):188-198. 3. Kuter DJ, Gouia I, Cordoba M, et al. Clinical burden of illness in patients with persistent or chronic primary immune thrombocytopenia treated with advanced therapies in the United States. Poster presented at: American Society of Hematology Annual Meeting & Exposition; December 7-10, 2024; San Diego, CA. 4. Cooper N, Morrison MA, Vladescu C, et al. Identification of occult cerebral microbleeds in adults with immune thrombocytopenia. Blood. 2020;136(25):2875-2880. 5. van Dijk WEM, Nap-van der Vlist MM, Knoop H, Schutgens REG. Possible targets to reduce fatigue in chronic immune thrombocytopenia patients – an explorative study. TH Open. 2022;6(4):e387-e395. 6. Hill QA, Newland AC. Fatigue in immune thrombocytopenia. Br J Haematol. 2015;170(2):141-149. 7. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (I-WISh): impact of ITP on health-related quality of life. Am J Hematol. 2021;96(2):199-207. 8. Newton JL, Reese JA, Watson SI, et al. Fatigue in adult patients with primary immune thrombocytopenia. Eur J Haematol. 2011;86(5):420-429. 9. Matzdorff A, Meyer O, Ostermann H, et al. Immune thrombocytopenia – current diagnostics and therapy: recommendations of a joint working group of DGHO, ӦGHO, SGH, GPOH, and DGTI. Oncol Res Treat. 2018;41(suppl 5):1-30. 10. Iron-Deficiency Anemia. National Heart, Lung, and Blood Institute (NIH). Updated March 24, 2022. Accessed May 9, 2025. 11. Terrell DR, Neunert CE, Cooper N, et al. Immune thrombocytopenia (ITP): current limitations in patient management. Medicina (Kaunas). 2020;56(12):667. 12. Saldanha A, Colella MP, Villaça PR, Thachil J, Orsi FA. The immune thrombocytopenia paradox: should we be concerned about thrombosis in ITP? Thromb Res. 2024;241:109109. 13. Vladescu C, Hart ACJ, Paul D, et al. Cognitive impairment in patients with immune thrombocytopenia. Blood. 2022;140(suppl 1):5553-5554. 14. Manfra A, Tun KM, Chang MJ, Wahi-Gururaj S. Oculomotor nerve palsy as a manifestation of immune thrombocytopenic purpura: a case report. Cureus. 2022;14(9):e29723. 15. Pongsakul A, Daniel A, Lochala R, Martin DE. Intracerebral hemorrhage in a patient with newly diagnosed immune thrombocytopenic purpura precipitated by a viral illness. Cureus. 2024;16(3):e57284. 16. Psaila B, Petrovic A, Page LK, Menell J, Schonholz M, Bussel JB. Intracranial hemorrhage (ICH) in children with immune thrombocytopenia (ITP): study of 40 cases. Blood. 2009;114(23):4777-4783. 17. Diyora B, Purandare A, Devani K, Kale P, Shah V, Patankar R. Life-threatening intracerebral hemorrhage in adult with ITP: challenging entity. Asian J Neurosurg. 2023;18(2):391-395.
MAT-GLB-2500852-v1.0-06/2025