- Article
- Source: Campus Sanofi
- Aug 2, 2025
Treatment Guidelines

ITP treatment guidelines for adults1-3
The ideal treatment for ITP varies between different age groups. Therefore, healthcare providers must consider the patient’s age when preparing a treatment plan. Below is a summary of ASH recommendations on how to treat ITP in adults.
ASH recommendations mainly cover primary immune thrombocytopenia guidelines, where the primary cause of ITP is unknown. In secondary ITP, the cause of the disease (eg, an infection or medication) is known and first-line treatment often addresses the pre-existing condition.
First-line ITP treatment1
Key decisions for healthcare providers treating ITP are criteria for admitting a patient to the hospital and when to start treatment.
Newly diagnosed patients with a platelet count below 20 (x109/L) without life-threatening bleeding should be admitted to the hospital, whilst patients with an established ITP diagnosis or a platelet count exceeding 20 (x109/L) can be treated at home.
Not all patients with ITP require medical interventions. Asymptomatic patients with non-life-threatening bleeding and a platelet count exceeding 30 (x109/L) can be managed with observation. In contrast, first-line treatment should be considered for all patients when their platelet count falls below 30 (x109/L).
Management of adult ITP patients with non-life-threatening bleeding1:
| Initial pharmacological intervention vs observation | ||
| Clinical criteria | Platelet count <30 (x109/L) in Newly diagnosed ITP patients who are asymptomatic or have minor mucocutaneous bleeding | Platelet count ≥30 (x109/L) in Newly diagnosed ITP patients who are asymptomatic or have minor mucocutaneous bleeding |
| Management recommendation | Start of first-line treatment | Observation |
| Hospital admission vs home management | ||
| Platelet count <20 (x109/L) in Newly diagnosed ITP patients who are asymptomatic or have minor mucocutaneous bleeding | Platelet count ≥20 (x109/L) in Newly diagnosed ITP patients who are asymptomatic or have minor mucocutaneous bleeding | |
| Inpatient treatment | Outpatient treatment | |
First-line treatments for ITP include corticosteroids, intravenous immunoglobulin (IVIg), and anti-D immunoglobulin. Corticosteroids are deemed a suitable first-line treatment for most ITP patients. Importantly, all first-line treatment decisions should consider the patient’s preferences.1,2,4
The impact of ITP on patients goes beyond platelet burden and can severely impact a person’s quality of life. The treatment therapies or treatment modalities of ITP can also adversely affect patients. For instance, corticosteroids can cause hypertension and negatively influence sleep and mental health.1,2,4
Treating healthcare providers should consider regularly assessing patients living with ITP and their health-related quality of life (HRQoL). Learn more about assessments of patients living with ITP. 1,2,4
Advanced therapy use for ITP
Some patients do not respond to corticosteroids or experience ITP for more than 3 months.1
For these patients, a change in the treatment plan should be considered. Second-line ITP treatment options include rituximab, splenectomy, and thrombopoietin receptor agonists (TPO-RA).1
The guidelines provide comprehensive considerations for selecting the best second-line treatments for ITP. Patients who are opposed to long-term medication may benefit from a splenectomy or treatment with rituximab. However, ITP patients can spontaneously go into remission within the first year,1 in which case a splenectomy should be avoided in this period. On the other hand, TPO-RAs might be a suitable option for patients who place a high value on achieving a durable response or avoiding surgery.1
In patients with additional risk factors, some treatments may elevate the risk of thrombosis and thromboembolism.5,6
Considerations influencing treatment discussions1:
- Adherence to medication
- Age of the patient
- Availability
- Comorbidities
- Cost
- Duration of the disease
- Frequency of bleeding
- Patient preferences
Overall, more treatment options are needed in ITP. Response rates and durability of current treatments can vary widely whilst some also have unfavourable side effect profiles or dosing regimens. Learn more about the future of ITP treatments.7,8
ITP treatment algorithm
Making a second-line treatment plan for ITP is complex as patient preferences and different clinical factors must be considered.1,2
This treatment algorithm for adult patients can help provide general guidance on managing persistent or first-line treatment-resistant ITP. 1,2
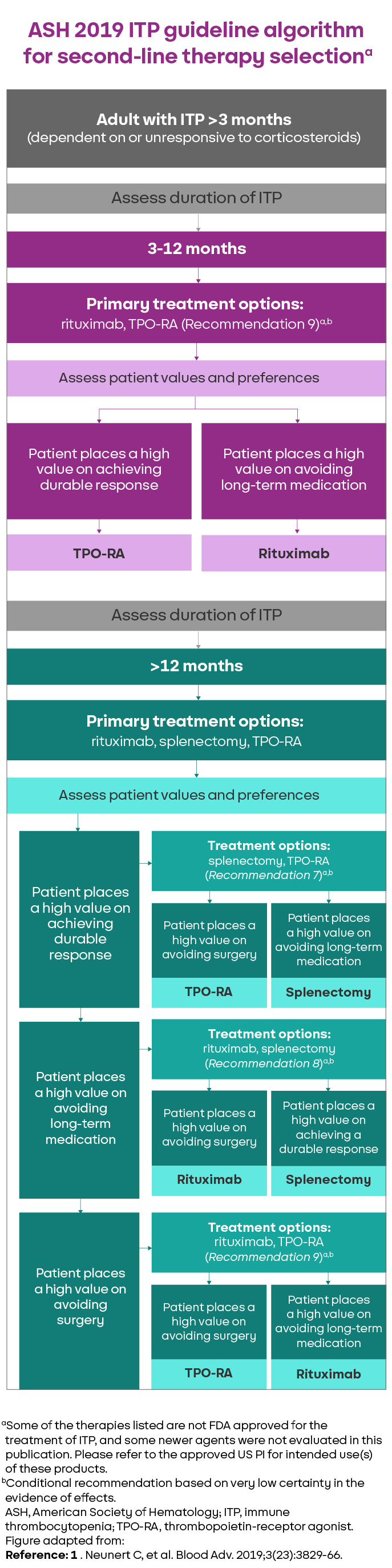
Figure 1. Algorithm for the selection of second-line therapy in adults with ITP. Selection of second-line therapy in adults with ITP should be individualised based on duration of disease and patient values and preferences. Other factors that may influence treatment decisions include frequency of bleeding sufficient to require hospitalisation or rescue medication, comorbidities, compliance, medical and social support networks, cost, and availability of treatments. Patient education and shared decision-making is encouraged. Numbered recommendations corresponding to each treatment option are provided.1
Limitations of the ASH ITP treatment guidelines for adults
The guidelines only cover patients who have been already diagnosed with ITP and exclude guidance on treatments approved after 2017 and patients who are pregnant or haemorrhaging.1
Do other ITP guidelines agree?
Guidelines for ITP can differ slightly between countries. However, most guidelines are aligned on treatment approaches, including2,6:
- An emphasis on incorporating patient preference into treatment decisions and discussing the potential impact of different treatments on quality of life.
- Acknowledging that preferences of patients with chronic ITP may evolve during the course of the disease and recommending ongoing discussions as a routine part of follow-up.
ASH, American Society of Hematology; IVIg, intravenous immunoglobulin; HRQoL, health-related quality of life; ITP, immune thrombocytopenic purpura.
References
1. Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3(23):3829-3866. 2. Matzdorff A, Meyer O, Ostermann H, et al. Immune thrombocytopenia – current diagnostics and therapy: recommendations of a joint working group of DGHO, ÖGHO, SGH, GPOH, and DGTI. Oncol Res Treat. 2018;41(suppl 5):1-30. 3. Cines DB, Bussel JB, Liebman HA, Luning Prak ET. The ITP syndrome: pathogenic and clinical diversity. Blood. 2009;113(26):6511-6521. 4. McMillan R, Bussel JB, George JN, Lalla D, Nichol JL. Self-reported health-related quality of life in adults with chronic immune thrombocytopenic purpura. Am J Hematol. 2008;83(2):150-154. 5. Dong Y, Xia Z, Zhou J, et al. Risk of thrombotic events in immune thrombocytopenia patients treated with thrombopoietic agents: a systematic review and meta-analysis. Thromb J. 2023;21(1):69. 6. Choi PY, Merriman E, Bennett A, et al. Consensus guidelines for the management of adult immune thrombocytopenia in Australia and New Zealand. Med J Aust. 2022;216(1):43-52. 7. Mingot-Castellano ME, Bastida JM, Caballero-Navarro G, et al. Novel therapies to address unmet needs in ITP. Pharmaceuticals (Basel). 2022;15(7):779. 8. Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381(10):945-955.
MAT-GLB-2500852-v1.0-06/2025