- Article
- Source: Campus Sanofi
- Aug 27, 2024
Can autoimmune type 1 diabetes be detected years before symptom onset?

Key Takeaway
Is the pathogenesis of autoimmune T1D poorly understood?
The pathogenesis of autoimmune T1D involves a complex interaction between the beta cells and immune system.1 It begins when the autoreactive T cells recognize and destroy the pancreatic beta cells. This leads to a critical decline in insulin levels, which in turn causes ineffective control of blood glucose levels. Eventually, the remaining beta cells become insufficient to maintain normal blood glucose reducing insulin secretion and leading to autoimmune T1D.2
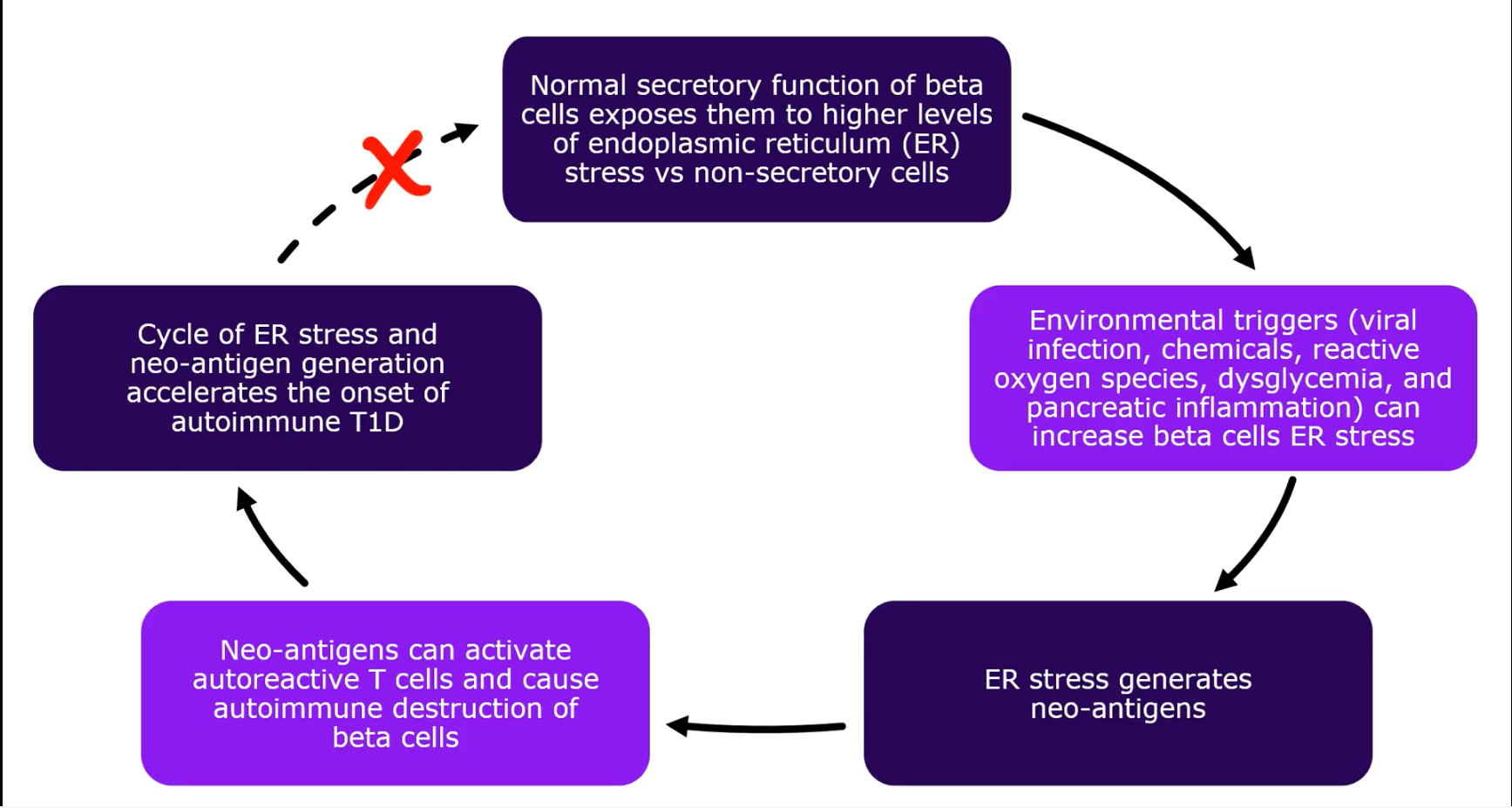
Lately, many autoantigens responsible for triggering immune-mediated destruction of beta cells have been identified; however, the triggering factors for this autoimmune response remain poorly understood.2,3
Please hit the play button below to understand one of the potential mechanisms behind the triggering of the autoimmune response
A potential mechanism for triggering autoimmune response2
Does the onset of autoimmune T1D begin long before symptoms appear?
In general, autoimmune T1D is a disease continuum that progresses sequentially through identifiable stages before symptoms appear. The rate of progression of T1D from the stage of autoimmune response to symptomatic disease varies among individuals and may take from few months to decades.3
Genetic susceptibility and genetic risk detection of autoimmune T1D
It is noteworthy that people living with other associated autoimmune diseases, such as celiac disease, autoimmune thyroid disease, are at an increased risk of developing autoimmune T1D than the general population.4 Shared genetic risk factors and immune system dysregulation are potentially implicated both in polyautoimmunity (occurrence of ≥2 autoimmune diseases in a single patient) and family autoimmunity (presence of ≥2 autoimmune diseases in members of a nuclear family) among individuals with autoimmune T1D.5
Currently, first- or second-degree relatives of individuals with autoimmune T1D or pediatric population are being screened for increased risk of developing autoimmune T1D in the research setting.3
For additional information on common genetic risk factors linked to autoimmune T1D, please read this article.
Does your patient have an existing autoimmune condition? Check for autoimmune type 1 diabetes risk!
What are the stages of autoimmune T1D?
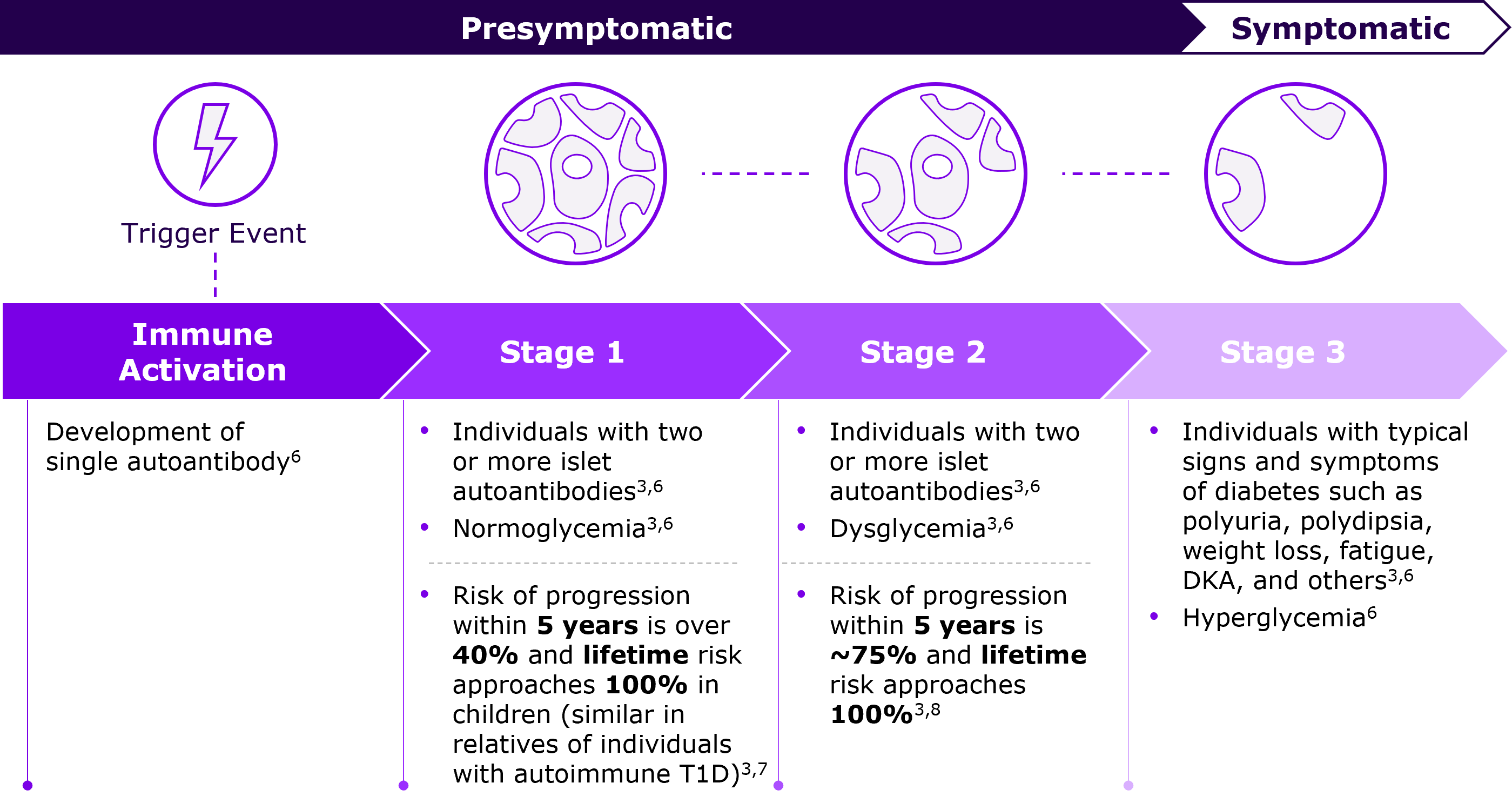
The Breakthrough T1D (formerly JDRF), the Endocrine Society, and the American Diabetes Association (ADA) have proposed three distinct stages of development and progression of autoimmune T1D, starting with the stage of activation of autoimmune response against the beta cells through symptomatic T1D.3
Progressive destruction of beta-cell function through different stages of autoimmune T1D3,6
In Stage 1, two or more autoantibodies against the pancreatic islets are detectible in the peripheral circulation which serve as a marker of autoimmunity. Beta-cell number and function begins to decline but are adequate to maintain normoglycemia.3
In Stage 2, progressive beta-cell damage compromises insulin production, and glycemic control cannot be maintained consistently, resulting in dysglycemia. Autoantibodies persist in the peripheral circulation.3
In Stage 3, beta-cell function is reduced such that blood glucose levels are consistently elevated and treatment with insulin is eventually required. Clinical symptoms of autoimmune T1D appear, including polyuria, polydipsia, weight loss, fatigue, and diabetic ketoacidosis (DKA).3
The below figure illustrates the three distinct stages of autoimmune T1D.
Can autoimmune T1D be identified before symptom onset?
Conventionally, autoimmune T1D is diagnosed after onset of clinical symptoms. However, latest research evidence on pathophysiological mechanisms leading to development and progression of T1D enable us to identify autoimmune T1D in its presymptomatic stages (Stage 1 and Stage 2 as described above).3
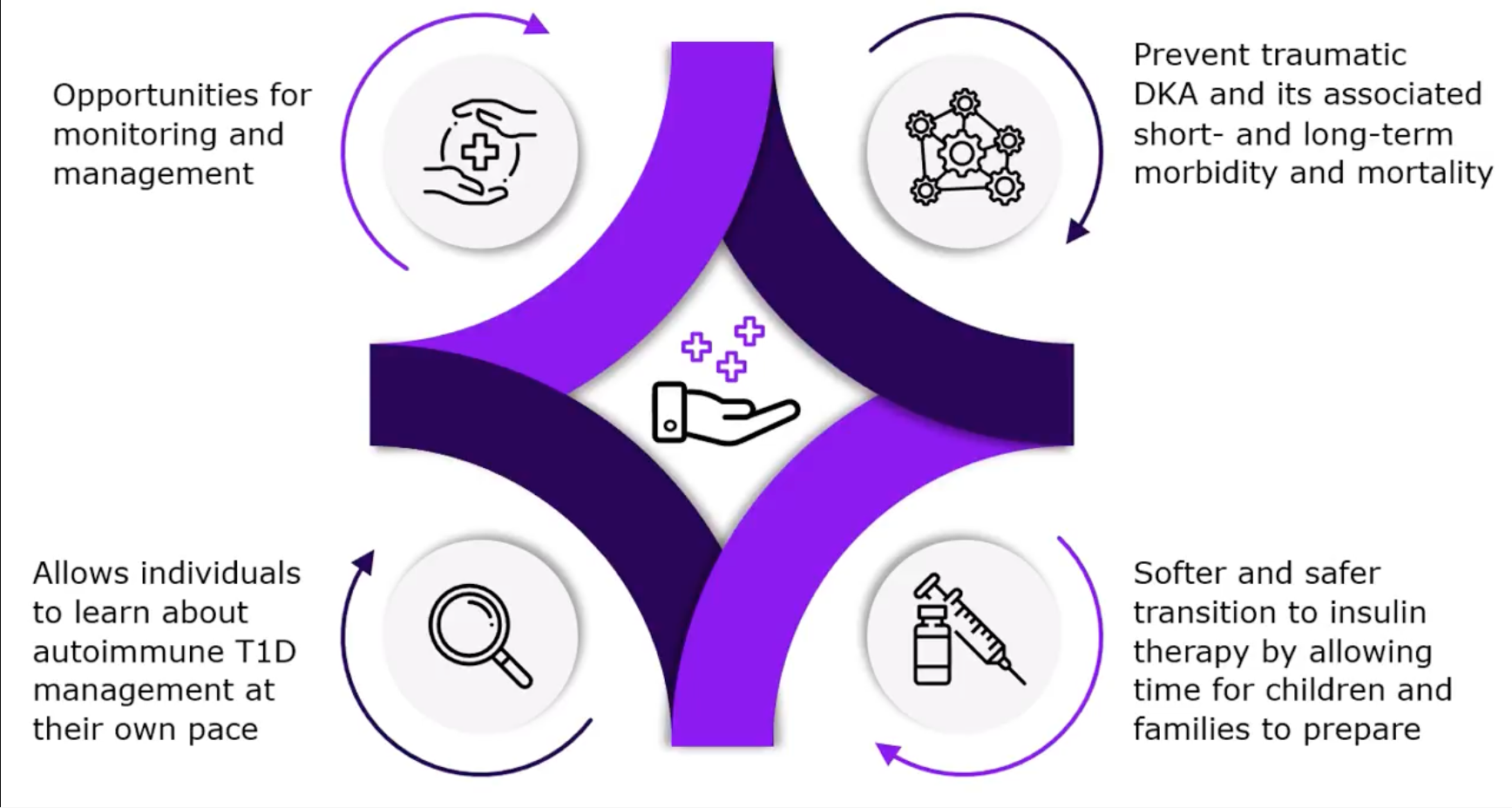
Early detection of presymptomatic stages through screening for autoantibodies provides us with an opportunity to intervene, to delay and ultimately prevent the symptomatic manifestation of autoimmune T1D.3
Early identification of individuals at risk of autoimmune T1D has a range of potential benefits6,9–11
Please click on the play button below to explore the potential benefits!
Early detection of autoimmune T1D is possible. You can identify patients at risk months to years before clinical symptoms appear!1-3
References
- DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391(10138):2449–2462.
- Marré ML, James EA, Piganelli JD. β cell ER stress and the implications for immunogenicity in type 1 diabetes. Front Cell Dev Biol. 2015;3:67.
- Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015;38(10):1964–1974.
- Barker JM. Clinical review: Type 1 diabetes-associated autoimmunity: natural history, genetic associations, and screening. J Clin Endocrinol Metab. 2006;91(4):1210–1217.
- Głowińska-Olszewska B, Szabłowski M, Panas P, et al. Increasing co-occurrence of additional autoimmune disorders at diabetes type 1 onset among children and adolescents diagnosed in years 2010-2018-single-center study. Front Endocrinol (Lausanne). 2020;11:476.
- Sims EK, Besser REJ, Dayan C, et al. Screening for type 1 diabetes in the general population: A status report and perspective. Diabetes. 2022;71(4):610–623.
- Ziegler AG, Rewers M, Simell O, et al. Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA. 2013;309:2473–2479.
- Krischer JP; Type 1 Diabetes TrialNet Study Group. The use of intermediate endpoints in the design of type 1 diabetes prevention trials. Diabetologia. 2013;56:1919–1924.
- Narendran P. Screening for type 1 diabetes: Are we nearly there yet? Diabetologia. 2019;62(1):24–27.
- Besser REJ, Bell KJ, Couper JJ, et al. ISPAD clinical practice consensus guidelines 2022: Stages of type 1 diabetes in children and adolescents. Pediatr Diabetes. 2022;23(8):1175–1187.
- Hummel S, Carl J, Friedl N, et al. Children diagnosed with presymptomatic type 1 diabetes through public health screening have milder diabetes at clinical manifestation. Diabetologia. 2023;66(9):1633–1642.
MAT-GLB-2404126-2.0-08/2024