- Article
- Source: Campus Sanofi
- Aug 28, 2024
Does your patient have an existing autoimmune condition? Check for autoimmune type 1 diabetes!

Key Takeaway
*Polyautoimmunity is the occurrence of ≥2 autoimmune diseases in a single patient; †Family autoimmunity presence of ≥2 autoimmune diseases in members of a nuclear family
Could autoantibodies serve as markers for autoimmunity in T1D?
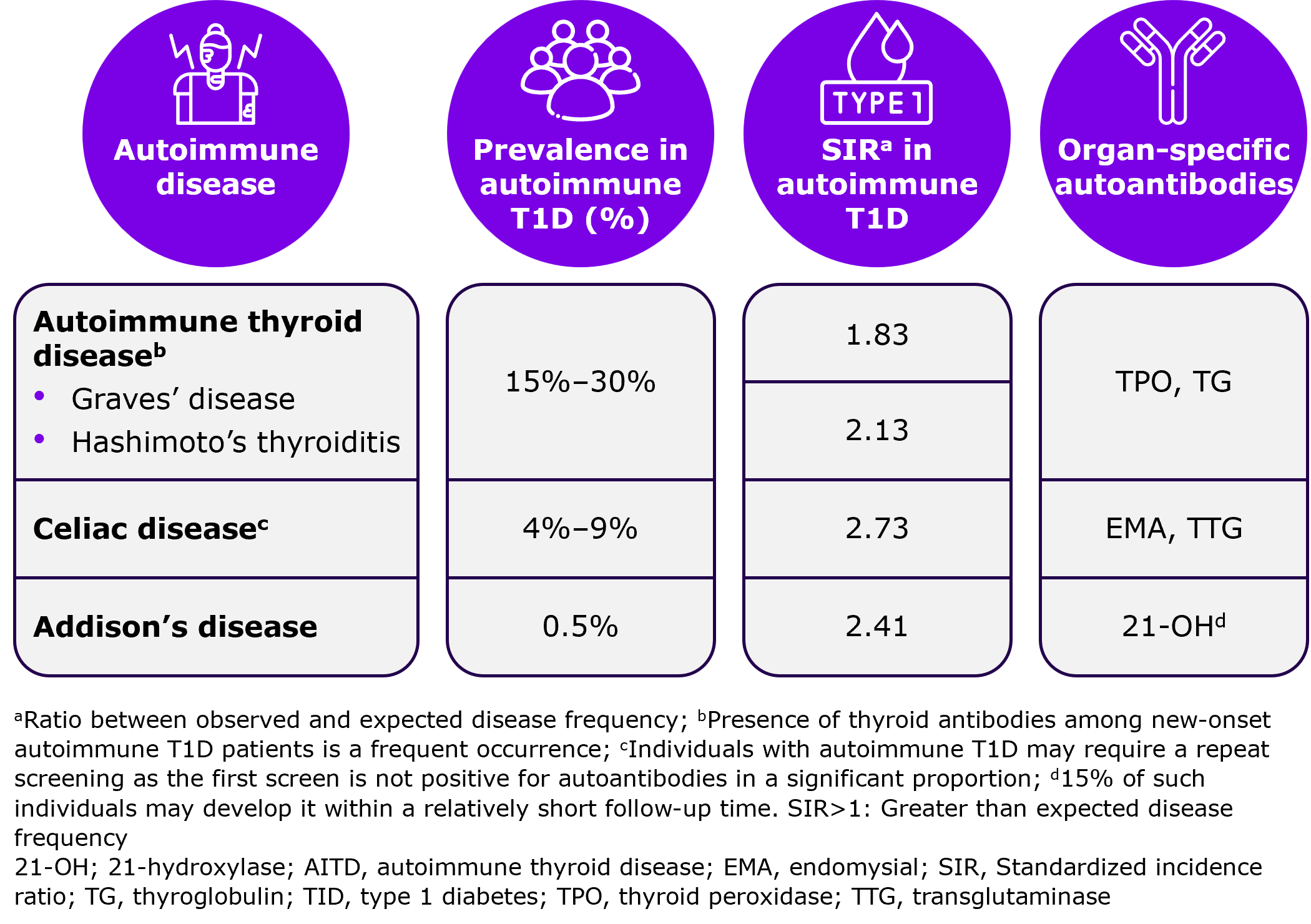
In some patients, autoimmune T1D is associated with the presence of additional autoimmune diseases, such as autoimmune thyroid disease, celiac disease, and Addison’s disease, which could lead to the production of organ-specific autoantibodies.1
Autoantibodies such as insulin autoantibodies (IAA), glutamic acid decarboxylase-65 (GAD-65), islet cell antigen 2 (IA-2), and islet cells autoantibodies (ICA), may be present for years prior to the diagnosis of autoimmune T1D and could serve as markers of autoimmune T1D.1
Do other associated autoimmune diseases frequently coexist with autoimmune T1D?
Concomitant autoimmune conditions may represent additional burden and complications in patients with autoimmune T1D.3,7 In the US, the prevalence of autoimmune diseases is higher in Caucasians and women and tends to rise with advancing age.7
Please refer to the below figure to know more about the prevalence of other associated autoimmune diseases linked with autoimmune T1D.
Prevalence of other associated autoimmune diseases linked with autoimmune T1D1,2
Is there a familial association between autoimmune T1D and other associated autoimmune diseases?
A familial association of T1D with other associated autoimmune diseases has been observed. Several genes linked to T1D risk also increase the chance of other associated autoimmune diseases.8
The inheritance pattern of autoimmune diseases is complex and involves multiple factors, including the consolidated impact of genotype and environmental triggers.2
Risk for autoimmune T1D
Autoimmune T1D puts first-degree relatives of patients at 1.6-times increased risk. A significant association for singleton siblings was found for autoimmune T1D (SIR = 2.14).2
Autoantibodies may develop sequentially. First-degree relatives expressing autoantibodies to IAA, GAD-65, and IA-2 had a 75% 5-year risk of diabetes vs 25% 5-year risk in relatives expressing only one of those autoantibodies.1 People diagnosed with Stage 2 autoimmune T1D have a near 100% lifetime chance of progression to Stage 3 autoimmune T1D, with 75% of them progressing within five years.9
Risk for other associated autoimmune diseases
Family autoimmunity is characterized by presence of ≥2 autoimmune diseases in members of a nuclear family.2 Autoimmune T1D also confers an increased risk of autoimmune diseases in first-degree relatives, with 8% and <6% developing autoimmune thyroid disease and celiac disease, respectively.1
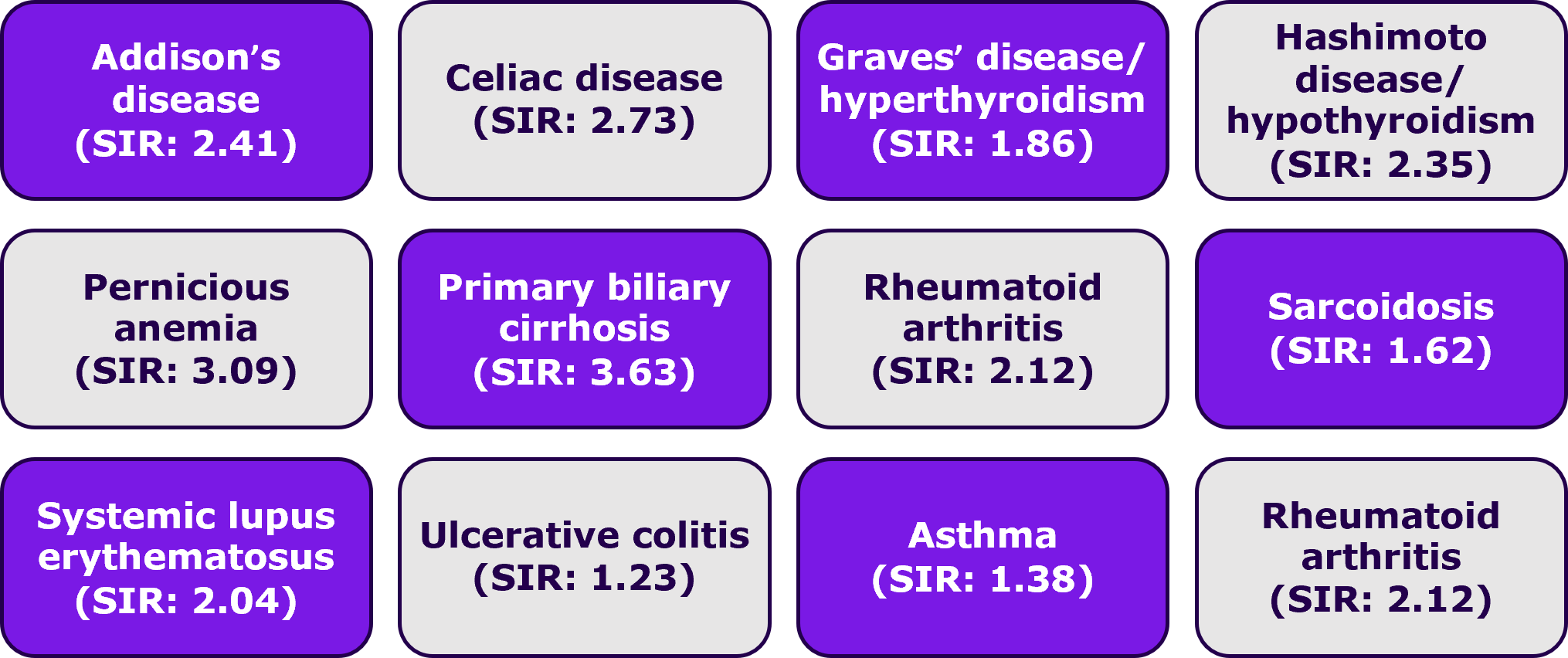
In a first population-level study that assessed the familial risks for T1D and a large number of other associated autoimmune diseases using MigMed database found that:8
T1D in offspring was associated with the following diseases in parents
Individuals with a first-degree relative with T1D have approximately 15-fold increased relative risk of developing T1D1
Do common genetic risk factors overlap for the autoimmune diseases?
Shared genetic risk factors and immune system dysregulation are potentially implicated both in polyautoimmunity and family autoimmunity among individuals with autoimmune T1D.2 Human leukocyte antigen (HLA) genotypes, PTPN22 gene, and cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) — all contribute to the complex interplay of genetic factors in autoimmune diseases that overlap with autoimmune T1D, as depicted in the below figure.1
| Genotype |
Disease association | Additional information |
|
HLA DR3-DQ2 & |
|
|
|
MHC class I chain related gene A Polymorphism of MIC-A (especially alleles 5 and 5.1) |
|
|
|
Polymorphism of PTPN22 gene, encoding LYP |
| NA |
|
CTLA-4 |
|
|
21-OH; 21-hydroxylase; AITD autoimmune thyroid disease; CTLA-4, cytotoxic T lymphocyte-associated antigen-4; HLA, human leukocyte antigen; LYP, lymphoid tyrosine phosphatase; MIC-A, MHC-I related gene; T1D, type 1 diabetes.
ADA guideline recommendations for screening of autoimmune diseases in autoimmune T1D
Individuals with an existing autoimmune disease are more prone to develop other associated autoimmune diseases.4-6,10
The 2024 ADA guidelines on Comprehensive Medical Evaluation and Assessment of Comorbidities recommend screening for autoimmune thyroid disease soon after a T1D diagnosis and periodically, thereafter. Additionally, screening for celiac disease is recommended in the presence of gastrointestinal symptoms, signs, laboratory manifestations, or suspicion of celiac disease.10
Screening for autoimmune T1D should be advised in individuals with other associated autoimmune diseases, given their higher risk than general population4‑6
References
- Barker JM. Clinical review: Type 1 diabetes-associated autoimmunity: natural history, genetic associations, and screening. J Clin Endocrinol Metab. 2006;91(4):1210–1217.
- Cardenas-Roldan J, Rojas-Villarraga A, Anaya JM. How do autoimmune diseases cluster in families? A systematic review and meta-analysis. BMC Med. 2013;11:73.
- Glowinska-Olszewska B, Szablowski M, Panas P, et al. Increasing co-occurrence of additional autoimmune disorders at diabetes type 1 onset among children and adolescents diagnosed in years 2010-2018-single-center study. Front Endocrinol (Lausanne). 2020;11:476.
- Ferrari SM, Fallahi P, Ruffilli I, Elia G, Ragusa F, Benvenga S, Antonelli A. The association of other autoimmune diseases in patients with Graves' disease (with or without ophthalmopathy): Review of the literature and report of a large series. Autoimmun Rev. 2019 Mar;18(3):287-292.
- Zelissen PM, Bast EJ, Croughs RJ. Associated autoimmunity in Addison's disease. J Autoimmun. 1995 Feb;8(1):121-30.
- Lauret E, Rodrigo L. Celiac disease and autoimmune-associated conditions. Biomed Res Int. 2013;2013:127589.
- Bao YK, Weide LG, Ganesan VC, et al. High prevalence of comorbid autoimmune diseases in adults with type 1 diabetes from the HealthFacts database. J Diabetes. 2019;11(4):273–279.
- Hemminki K, Li X, Sundquist J, Sundquist K. Familial association between type 1 diabetes and other autoimmune and related diseases. Diabetologia. 2009;52(9):1820-8.
- Besser REJ, Bell KJ, Couper JJ, et al. ISPAD clinical practice consensus guidelines 2022: Stages of type 1 diabetes in children and adolescents. Pediatr Diabetes. 2022;23:1175-87.
- American Diabetes Association Professional Practice C. 4. Comprehensive medical evaluation and assessment of comorbidities: Standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S52–S76.
MAT-GLB-2404125-2.0-08/2024