- Article
- Source: Campus Sanofi
- Aug 7, 2025
Defining ITP

The complex immune dysregulation of ITP can impact platelet counts, bleeding, and HRQoL.1,3-6
In ITP, dysregulation of immune pathways results in increased platelet destruction and decreased platelet production.7
Bleeding occurs in around 60% of patients. Bleeding symptoms vary and can include8:
Petechiae and purpura, usually on the extremities1,9
Heavy menstrual bleeding1
Bleeding blisters and epistaxis1,9
Intracranial haemorrhage8
Severe bleeding occurs in 7% to 10% of adult patients and is typically correlated with lower platelet counts.10,11
Some ITP patients may experience systemic symptoms, including fatigue, fever, tachycardia, and cognitive effects, such as headaches and memory impairment.1,12-14
Treatment of ITP typically focuses on managing primary symptoms such as petechiae, purpura, and bleeding. However, patients with ITP often experience other symptoms such as fatigue and difficulties with memory and concentration that can profoundly affect their quality of life. That is why it is important to use treatment strategies that help improve HRQoL in ITP patients.1,12-14
Purpura and petechiae in ITP
ITP is an autoimmune blood disorder where easy bruising, petechiae and purpura often appear as common symptoms typically in lower extremities. Petechiae and purpura occur due to bleeding under the skin or mucous membranes.15,16
Petechiae in thrombocytopenia
Petechiae are small, non-blanching red or purple pinpoint lesions, usually less than 2 mm, that appear on the skin and mucous membranes. Petechial rashes result from bleeding into the skin’s dermal layer.15,17
Purpura in thrombocytopenia
Purpura refers to larger areas of cutaneous bleeding, which appear as purple or red patches on the skin that measure greater than 2 mm in size.15,17
In patients with ITP, purpura can appear due to even minor trauma or spontaneously due to low platelet levels. Purpura can also appear in mucosal membranes such as the hard palate, nasal septum, or gums, which can lead to bleeding gums.15,16,18
Other ITP bleeding symptoms and complications of thrombocytopenia
A low platelet count can lead to certain types of bleeding symptoms in ITP patients, including nose bleeds (epistaxis), gum bleeds (gingival), mouth blood blisters, blood in urine or stools, and heavy menstrual bleeding.9,19
Platelet levels <10,000/μL could be associated with spontaneous widespread haematomas, and severe bleeding in ITP usually occurs when the platelet count is <10 (x109/L). Severe bleeding can manifest as intracranial haemorrhages, gastrointestinal tract bleeds, and macroscopic haematuria. In some studies, severe bleeding occurred in approximately 7% to 10% of adult patients and typically correlated with lower platelet counts.10-12,16,20,21
ITP and intracranial haemorrhaging (brain bleed)
Intracranial haemorrhaging (ICH) is a rare and serious complication of ITP. The incidence of ICH in ITP patients is 1.54% in all ages.19,20,22,23
ICH symptoms that are a cause for concern include headache, persistent vomiting, altered mental status, and seizures. Risk factors for ICH include extremely low platelet counts of <10,000/μL, head trauma, antiplatelet medication use, and severe bleeding.19,20,22,23
The symptoms of ITP go beyond bleeding
Learn more about the less visible symptoms of ITP and how they impact ITP patients’ quality of life.
Primary ITP is a diagnosis of exclusion7,24,25
- Platelet counts <100,000/μL can indicate ITP
- Platelet counts <50,000/μL can indicate severe thrombocytopenia
But the lack of a specific test means other potential causes of thrombocytopenia must be ruled out7,24,26,27
Causes of secondary ITP include7,24,26,27:
- Chronic lymphocytic leukaemia (CLL)
- Helicobacter pylori infection
- COVID-19 infection
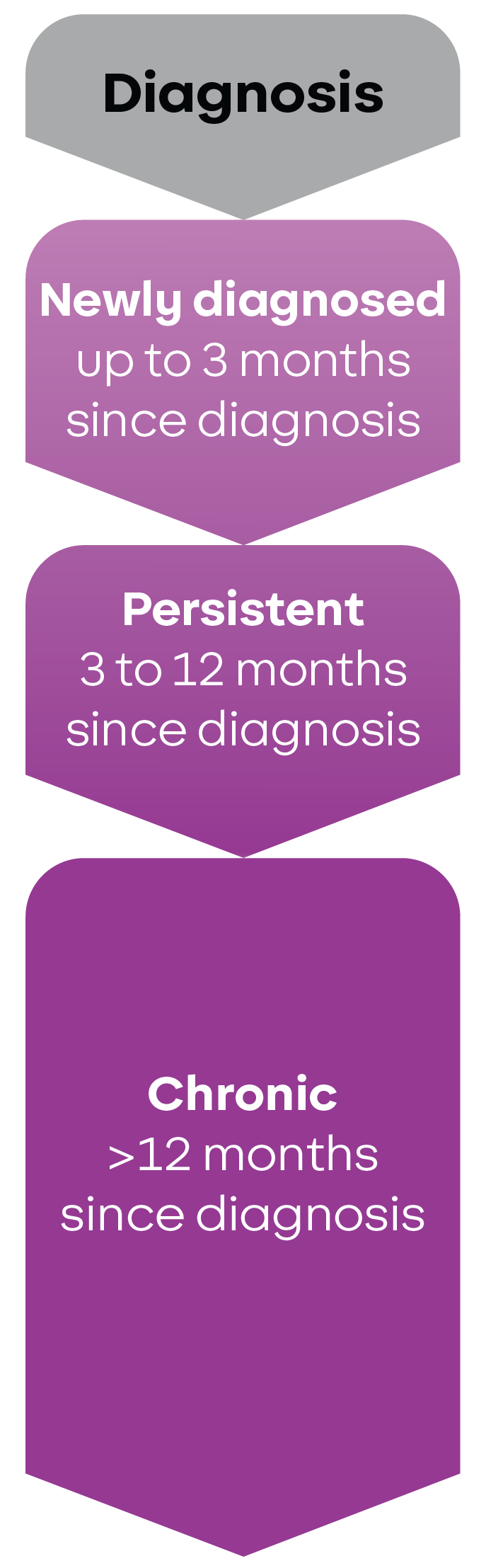
ITP is further classified as either newly diagnosed, persistent, or chronic27:
References
1. Cooper N, Kruse A, Kruse C, et al. Immune thrombocytopenia (ITP) World Impact Survey (iWISh): patient and physician perceptions of diagnosis, signs and symptoms, and treatment. Am J Hematol. 2021;96(2):188-198. 2. Kuter DJ, Gouia I, Cordoba M, et al. Clinical burden of illness in patients with persistent or chronic primary immune thrombocytopenia treated with advanced therapies in the United States. Poster presented at: American Society of Hematology Annual Meeting & Exposition; December 7-10, 2024; San Diego, CA. 3. Andreescu M. The link between immune thrombocytopenia and the cytokine profile: a bridge to new therapeutical targets. Front Hematol. 2023;2:1191178. 4. Qiao J, Liu Y, Li X, et al. Elevated expression of NLRP3 in patients with immune thrombocytopenia. Immunol Res. 2016;64(2):431-437. 5. Schifferli A, Cavalli F, Godeau B, et al. Understanding immune thrombocytopenia: looking out of the box. Front Med (Lausanne). 2021;8:613192. 6. McMillan R, Bussel JB, George JN, Lalla D, Nichol JL. Self-reported health-related quality of life in adults with chronic immune thrombocytopenic purpura. Am J Hematol. 2008;83(2):150-154. 7. Cooper N, Ghanima W. Immune thrombocytopenia. N Engl J Med. 2019;381(10):945-955. 8. Audia S, Bonnotte B. Emerging therapies in immune thrombocytopenia. J Clin Med. 2021;10(5):1004. 9. Kistangari G, McCrae KR. Immune thrombocytopenia. Hematol Oncol Clin North Am. 2013;27(3):495-520. 10. Piel-Julian M-L, Mahévas M, Germain J, et al. Risk factors for bleeding, including platelet count threshold, in newly diagnosed immune thrombocytopenia adults. J Thromb Haemost. 2018;16(9):1830-1842. 11. Neunert C, Noroozi N, Norman G, et al. Severe bleeding events in adults and children with primary immune thrombocytopenia: a systematic review. J Thromb Haemost. 2015;13(3):457-464. 12. Pietras NM, Gupta N, Justiz Vaillant AA, Pearson-Shaver AL. Immune Thrombocytopenia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 5, 2024. 13. van Dijk WEM, Nap-van der Vlist MM, Knoop H, Schutgens REG. Possible targets to reduce fatigue in chronic immune thrombocytopenia patients - an explorative study. TH Open. 2022;6(4):e387-e395. 14. Kuter DJ, Khan U, Maruff P, Daak A. Cognitive impairment among patients with chronic immune thrombocytopenia. Br J Haematol. 2024;205(1):291-299. 15. Rodeghiero F, Michel M, Gernsheimer T, et al. Standardization of bleeding assessment in immune thrombocytopenia: report from the International Working Group. Blood. 2013;121(14):2596-2606. 16. Zainal A, Salama A, Alweis R. Immune thrombocytopenic purpura. J Community Hosp Intern Med Perspect. 2019;9(1):59-61. 17. McGrath A, Barrett MJ. Petechiae. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 4, 2023. 18. Kayal L, Jayachandran S, Singh K. Idiopathic thrombocytopenic purpura. Contemp Clin Dent.2014;5(3):410-414. 19. Immune Thrombocytopenia. The National Organization for Rare Disorders (NORD). Updated July 12, 2022. Accessed May 9, 2025. 20. Madkhali MA. Recent advances in the management of immune thrombocytopenic purpura (ITP): a comprehensive review. Medicine (Baltimore). 2024;103(3):e36936. 21. Arnold DM. Bleeding complications in immune thrombocytopenia. Hematology Am Soc Hematol Educ Program. 2015;2015:237-242. 22. Pongsakul A, Daniel A, Lochala R, Martin DE. Intracerebral hemorrhage in a patient with newly diagnosed immune thrombocytopenic purpura precipitated by a viral illness. Cureus. 2024;16(3):e57284. 23. Diyora B, Purandare A, Devani K, Kale P, Shah V, Patankar R. Life-threatening intracerebral hemorrhage in adult with ITP: challenging entity. Asian J Neurosurg. 2023;18(2):391-395. 24. Rovó A, Cantoni N, Samii K, et al. Real-world impact of primary immune thrombocytopenia and treatment with thrombopoietin receptor agonists on quality of life based on patient-reported experience: results from a questionnaire conducted in Switzerland, Austria, and Belgium. PLoS One. 2022;17(4):e0267342. 25. Williamson DR, Albert M, Heels-Ansdell D, et al. Thrombocytopenia in critically ill patients receiving thromboprophylaxis: frequency, risk factors, and outcomes. Chest. 2013;144(4):1207-1215. 26. Kewan T, Gunaratne TN, Mushtaq K, et al. Outcomes and management of immune thrombocytopenia secondary to COVID-19: Cleveland clinic experience. Transfusion. 2021;61(7):2014-2018. 27. Rodeghiero F, Stasi R, Gernsheimer T, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009;113(11):2386-2393.
MAT-GLB-2500852-v1.0-06/2025