- Article
- Source: Campus Sanofi
- Dec 1, 2025
Importance of early screening for autoimmune T1D in children and adolescents

Key takeaway
Burden of T1D in children and adolescents
The incidence of T1D has risen significantly over the past five decades with those <18 years most impacted.2
Notably, 90% of children who develop T1D are found in the general population and lack a family history of T1D.2
The most common type of diabetes in childhood and adolescence is immune-mediated.3 Children with autoimmune T1D face three times higher hospitalization rates than their healthy peers and they are more prone to depression, anxiety, psychological distress, and eating disorders.2 Long-term glycemic control is often suboptimal, with fear of hypoglycemia being a major limiting factor.2
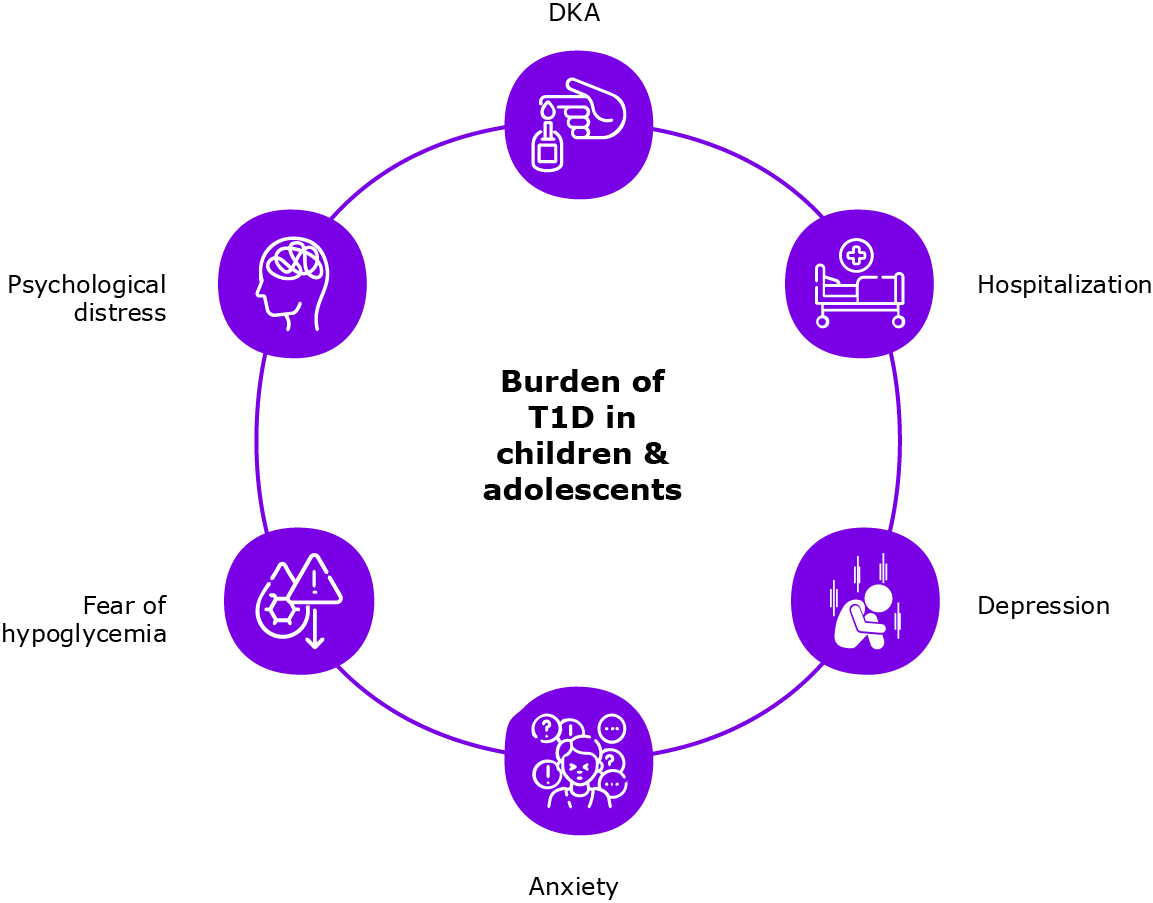
In a large majority of children, autoimmune T1D diagnosis is associated with DKA, a clinical emergency.2 DKA can be associated with poor metabolic control over a long term, cerebral edema, extended hospitalization, excessive costs, and high mortality rates.2
Screening children can help reduce autoimmune T1D burden
Children who develop autoantibodies and progress to autoimmune T1D early in life have reduced functional beta cell mass and higher rates of DKA at diagnosis.4 DKA awareness campaigns effectively reduce DKA at autoimmune T1D onset, but large-scale implementation of prevention campaigns remains challenging.2
Islet autoantibodies screening potentially prevents DKA by effectively identifying individuals at a higher risk of developing autoimmune T1D.1,5 Screening also provides an opportunity for patient and caregiver education and glucose monitoring in the high-risk cohort.1 Closely monitored children have significantly lower DKA rates.6
Early screening can, thus, help prevent DKA by early identification of children with autoantibodies and their close monitoring.7 However, autoantibodies are often screened later in the disease trajectory.8 Furthermore, it has been observed that frequency of screening is higher in children with first-degree relatives with autoimmune T1D that in those without.9 Establishing larger population screening can help identify at-risk children and those who might benefit from preventive/ immunomodulatory treatments.10
Cheaper autoantibody screening tests along with potentially reduced incidence and economic impact of diabetes complications can make early screening for autoimmune T1D cost effective.2
The high rates of DKA at diagnosis in adolescence makes screening crucial in this age group.1
One time screening at 10 years of age during adolescence is shown to be highly sensitive with a high positive predictive value.1
Real world evidence for screening in children and adolescents
| Studies | Outcomes | n | Screened children found positive for islet autoantibodies | n | Non-screened children | P-value |
| German BABYDIAB and the Munich Family Study*11 |
Prevalence of DKA |
65 |
3.3% |
15,359 |
29.1% |
<0.001 |
|
HbA1c |
71 |
8.6% |
20,024 |
11.0% |
< 0.001 | |
|
Blood glucose levels, mmol/L |
48 |
19.01 |
14,022 |
23.86 |
0.005 | |
|
Hospitalization duration, days |
53 |
11.4 |
21,170 |
14.9 |
0.005 | |
|
Blood pH levels |
65 |
7.39 |
15,359 |
7.31 |
<0.001 | |
| DAISY12 |
Outcomes |
Children diagnosed with diabetes through screening and follow-up program |
Children concurrently diagnosed with diabetes in the community |
P-value | ||
|
HbA1c at diagnosis |
7.2% |
10.9% |
<0.0001 | |||
|
Hospitalization rate |
3.3% |
44% |
<0.0001 | |||
Learn how early detection of autoimmune T1D could reduce the risk of DKA
Guideline recommendations for screening of children and adolescents
Recent consensus guidelines recommend screening at ages 2 and 6 for optimal prediction of development of clinical autoimmune T1D by the age of 15 years. However, this approach tends to miss a subset of younger infants and toddlers (<2 years of age) and adolescents (10–18 years) who may be at risk of developing autoimmune T1D.13
If the initial screening window of 2 to 6 years is missed, providers should screen children who they believe are suitable candidates any time thereafter.13
The ISPAD 2024 consensus document for screening individuals with single (at-risk) and multiple (early-stage autoimmune T1D) islet autoantibody positivity provides the following expert clinical advice for screening individuals with islet autoantibody–positive pre-stage 3 T1D:14
- Surveillance frequency should depend on the risk of progression, with more frequent monitoring offered to children at higher risk of progression
- Screening for islet autoantibodies repeated twice during childhood may provide the most cost-effective means of identifying those who will develop autoimmune T1D. Optimal ages for screening may depend on background population risk
- Screening should be coupled with education and metabolic surveillance programs for those identified with islet autoantibodies
- All families need to be counseled about the expected progression to clinical diagnosis of autoimmune T1D, how to cope with the often-unexpected diagnosis of early-stage autoimmune T1D, options for glycemic monitoring, and how to identify signs and symptoms of hyperglycemia, and have a team to contact
The ADA 2025 guidelines recommend that the first autoantibody-positive test be confirmed with a second test within 3 months, preferably in a laboratory that meets the performance standards set by the Islet Autoantibody Standardization Program (IASP).3
Learn what is the need to identify risk of developing autoimmune T1D
Role of HCPs in addressing psychological impact of autoimmune T1D in families and caregivers
Screening for autoimmune T1D could cause significant psychological stress in children diagnosed with pre-symptomatic T1D and their parents.2 Early detection of autoimmune T1D necessitates HCPs to offer follow-up education and counseling to individuals and their families to manage stress, anxiety, and psychological issues during screening, monitoring, and potential treatment.13
Research indicates that providing education to families with children diagnosed with early pre-symptomatic stages of autoimmune T1D improves their quality of life and reduces parental stress at clinical autoimmune T1D.13
Learn more about psychosocial support for patients identified at risk or at early stage autoimmune T1D
References
- Ghalwash M, Anand V, Lou O, et al. Islet autoantibody screening in at-risk adolescents to predict type 1 diabetes until young adulthood: A prospective cohort study. Lancet Child Adolesc Health. 2023;7(4):261–268. doi:10.1016/S2352-4642(22)00350-9.
- Cherubini V, Chiarelli F. Autoantibody test for type 1 diabetes in children: are there reasons to implement a screening program in the general population? A statement endorsed by the Italian Society for Paediatric Endocrinology and Diabetes (SIEDP-ISPED) and the Italian Society of Paediatrics (SIP). Ital J Pediatr. 2023;49(1):87. doi:10.1186/s13052-023-01438-3.
- American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2025. Diabetes Care. 2025;48(Supplement 1):S27–S49. doi:10.2337/dc25-S002.
- Felton JL, Redondo MJ, Oram RA, et al. Islet autoantibodies as precision diagnostic tools to characterize heterogeneity in type 1 diabetes: A systematic review. Commun Med (Lond). 2024;4(1):66. doi:10.1038/s43856-024-00478-y.
- Besser REJ, Bell KJ, Couper JJ, et al. ISPAD clinical practice consensus guidelines 2022: Stages of type 1 diabetes in children and adolescents. Pediatr Diabetes. 2022;23(8):1175–1187. doi:10.1111/pedi.13410.
- Simmons KM, Youngkin E, Alkanani A, et al. Screening children for type 1 diabetes-associated antibodies at community health fairs. Pediatr Diabetes. 2019;20(7):909–914. doi:10.1111/pedi.12902.
- Peters A. Screening for autoantibodies in type 1 diabetes: A Call to Action. J Fam Pract. 2021;70(6S):S47–S52. doi:10.12788/jfp.0223.
- Bertolini M, Duchateau D, Mikkelsen K, et al. Experiences and perspectives related to autoantibody screening of people at risk for type 1 diabetes. Poster 550. Presented at: The International Society for Pediatric and Adolescent Diabetes (ISPAD) 2024 Annual Conference; October 16, 2024; Lisbon, Portugal.
- Hood K, Agardh D, Ebekozien O, et al. Family ties and screening whys: Decisions in islet autoantibody testing for type 1 diabetes. Oral presentation 62. Presented at: The International Society for Pediatric and Adolescent Diabetes (ISPAD) 2024 Annual Conference; October 17, 2024; Lisbon, Portugal.
- Serra-Caetano J, Cardoso R, Dinis, I, et al. Type 1 diabetes screening in a pediatric population – lessons learned on a daily practice perspective. Poster 296. Presented at: The International Society for Pediatric and Adolescent Diabetes (ISPAD) 2024 Annual Conference; October 16, 2024; Lisbon, Portugal.
- Winkler C, Schober E, Ziegler AG, Holl RW. Markedly reduced rate of diabetic ketoacidosis at onset of type 1 diabetes in relatives screened for islet autoantibodies. Pediatr Diabetes. 2012;13(4):308–313. doi:10.1111/j.1399-5448.2011.00829.x.
- Barker JM, Goehrig SH, Barriga K, et al. Clinical characteristics of children diagnosed with type 1 diabetes through intensive screening and follow-up. Diabetes Care. 2004;27(6):1399–1404. doi:10.2337/diacare.27.6.1399.
- Moore DJ, Leibel NI, Polonsky W, et al. Recommendations for screening and monitoring the stages of type 1 diabetes in the immune therapy era. Int J Gen Med. 2024;17:3003–3014. doi:10.2147/IJGM.S438009.
- Haller MJ, Bell KJ, Besser REJ, et al. ISPAD clinical practice consensus guidelines 2024: Screening, staging, and strategies to preserve beta-cell function in children and adolescents with type 1 diabetes. Horm Res Paediatr. 2024. doi:10.1159/000543035.
MAT-GLB-2503433-2.0 - 12/2025