- Article
- Source: Campus Sanofi
- Jun 19, 2025
The pathophysiology of autoimmune type 1 diabetes
Pathogenesis of autoimmune T1D
The heterogeneous pathogenesis of autoimmune T1D is characterised by factors related to a person's genetics and their environment. Whilst key autoantigens have been identified, the initial triggers of the autoimmune T1D immune response remain uncertain.3
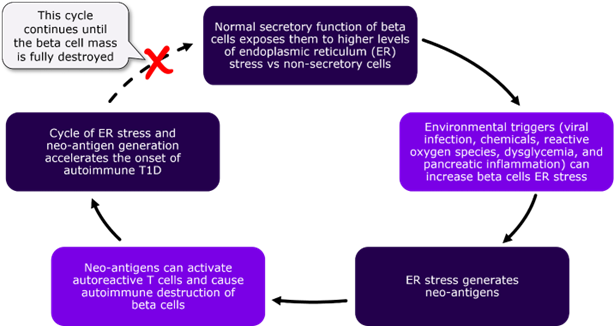
Autoimmunity and beta-cell destruction
The pathogenesis of autoimmune T1D begins when autoreactive T cells recognize and destroy pancreatic beta cells. This leads to a critical decline in insulin levels, which in turn causes ineffective control of blood glucose levels. Eventually, the remaining beta cells become insufficient to maintain normal blood glucose, reducing insulin secretion and leading to autoimmune T1D.4
Autoantigens and immune response
Autoimmune T1D patient´s immune system erroneously identifies specific beta cell components as autoantigens and attacks them.5 These T1D autoantigens can include6
- insulin B chain peptide (11-23)
- other beta-cell components such as GAD65, an enzyme associated with secretory vesicles
- protein phosphatase like IA-2
The presence of autoantibodies against these antigens serves as an important biomarker for disease progression, which is exponentially increased by any additional autoantibodies.6 Early detection of presymptomatic stages through screening for autoantibodies provides us with an opportunity to intervene, delay, and potentially prevent the symptomatic manifestation of autoimmune T1D.2
A potential mechanism for triggering autoimmune response4
.png)
Genetic susceptibility
When it comes to genetic factors, autoimmune T1D is strongly associated with specific HLA class II chain alleles which confer a higher risk for autoimmune T1D development.6
It is noteworthy that people living with other associated autoimmune diseases, such as celiac disease and autoimmune thyroid disease, are at an increased risk of developing autoimmune T1D than the general population.7
Does your patient have an existing autoimmune condition? Learn more about genetic risk factors linked to autoimmune T1D.
Metabolic consequences of insulin deficiency
The destruction of pancreatic beta-cells due to autoimmune T1D results in insulin deficiency. Insulin deficiency, coupled with increased counterregulatory hormones, triggers the release of free fatty acids from adipose tissue. These fatty acids are then oxidized in the liver to form ketone bodies, leading to diabetic ketoacidosis (DKA), which ultimately causes worsening of hyperglycemia.8 DKA is a life-threatening condition often associated with high mortality, morbidity, and healthcare expenditure.9 Early screening and detection of autoimmune T1D is therefore crucial for preventing DKA.
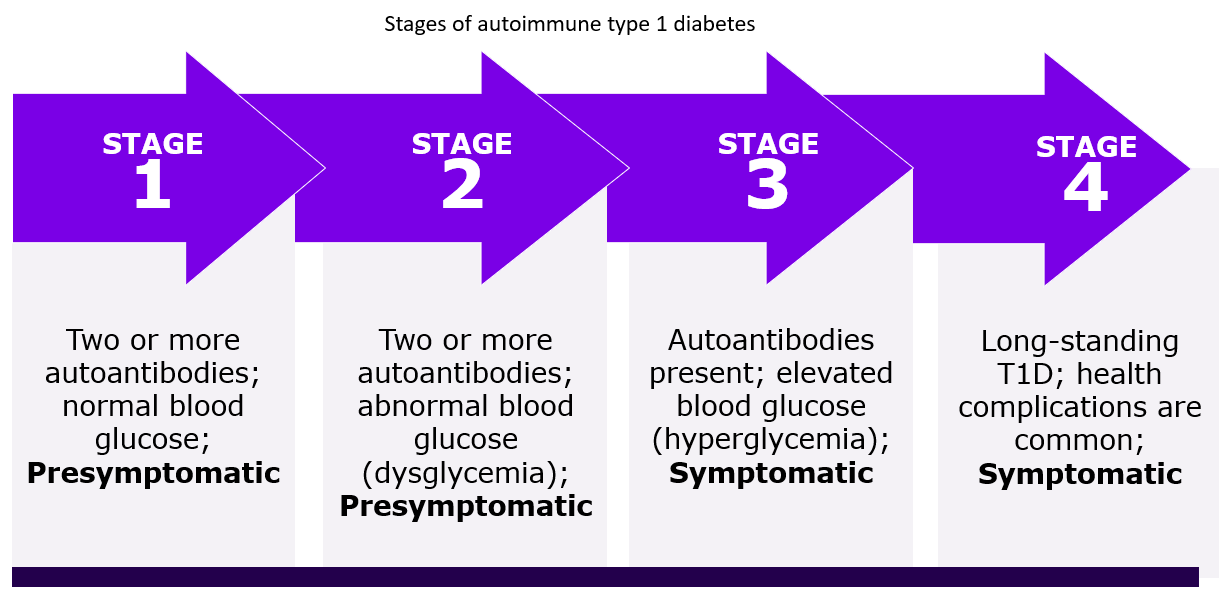
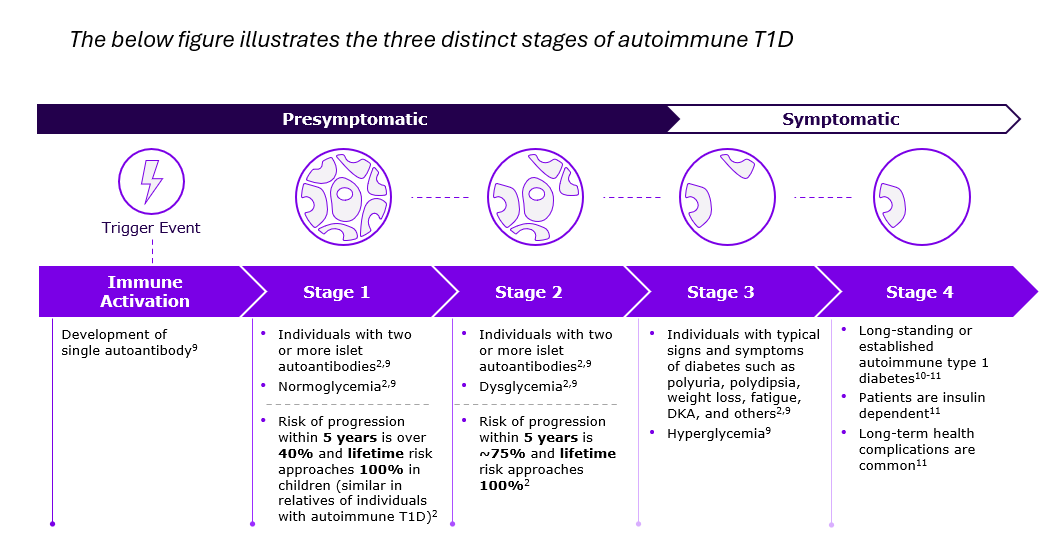
Stages of autoimmune T1D progression
There is a trigger event that initiates the pathogenesis of autoimmune T1D before it progresses through four stages and eventually results in symptomatic autoimmune T1D. An initial immune response occurs during this trigger event with the development of a single autoantibody. As soon as additional autoantigens are detected, the number of beta cells is already shrinking. However, the pace at which autoimmune T1D progresses from the first autoimmune reaction to symptomatic disease varies from individual to individual and can take anywhere from a few months to decades.2,9
.png)
Stage 1. Early autoimmunity and beta-cell decline
The first stage of a beginning autoimmunity is characterized by the presence of two or more autoantibodies against the pancreatic islets in the peripheral circulation. In this stage the functional impairment and reduction of beta-cells is already in progress, but the number is still sufficient to maintain normoglycemia. That is why no symptoms are apparent yet.2
Stage 2. Progressive beta-cell dysfunction
In stage 2, the destruction of the beta-cells progressively increases, resulting in the decrease of insulin production. Glycaemic control can no longer be maintained, which eventually leads to dysglycemia. Although still pre-symptomatic, the autoantibodies remain detectable in the peripheral circulation at this stage as a biomarker for autoimmunity.2
Stage 3. Clinical symptoms and insulin dependence
At this stage, the destruction of the beta-cells has reached a degree at which insulin production is no longer sufficient to keep the blood sugar stable. Patients at this stage now show the typical clinical symptoms of autoimmune T1D, such as polyuria, polydipsia, weight loss, fatigue, and diabetic ketoacidosis (DKA). Hyperglycemia also occurs at this point, which makes an insulin medication unavoidable.2
Stage 4. Long-standing autoimmune T1D
At stage 4, patient has long-standing autoimmune T1D after living with the condition for several years and is insulin dependent.10-11 Long-term health complications are common, and two or more autoantibodies may or may not be detected in the blood at stage 4 autoimmune T1D.11
Early detection and progression of autoimmune T1D
Due to the latest research evidence on pathophysiological mechanisms in the development of autoimmune T1D, it is now possible to screen patients in the presymptomatic stages (1 and 2) for suspicious autoantibodies. This provides the opportunity to intervene, delay and ultimately prevent the natural progression of autoimmune T1D, preserving beta cell function.2,12
.png)
Early identification of autoimmune T1D
Currently, first- or second-degree relatives of individuals with autoimmune T1D or pediatric population are being screened for increased risk of developing autoimmune T1D in the research setting.2 The improved understanding of the development and progression of autoimmune T1D enables early detection, utilising autoantibody screenings as a primary tool. It opens a variety of possibilities for patients and their relatives as well as for HCPs in their care.13
Learn more about how autoantibodies can be used to screen for T1D
References
- Popoviciu MS, Kaka N, Sethi Y, Patel N, Chopra H, Cavalu S. Type 1 Diabetes Mellitus and Autoimmune Diseases: A Critical Review of the Association and the Application of Personalized Medicine. J Pers Med. 2023;13(3):422. doi:10.3390/jpm13030422.
- Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015;38(10):1964-1974. doi:10.2337/dc15-1419.
- Rewers M, Ludvigsson J. Environmental risk factors for type 1 diabetes. Lancet. 2016;387(10035):2340-2348. doi:10.1016/S0140-6736(16)30507-4.
- Marré ML, James EA, Piganelli JD. β cell ER stress and the implications for immunogenicity in type 1 diabetes. Front Cell Dev Biol. 2015;3:67. doi:10.3389/fcell.2015.00067.
- Owens-Collins S. Beta Cell Regulation, Function, Dysfunction and Eventual Destruction in Type 1 Diabetes. IntechOpen eBooks. Published online May 15, 2023. doi:10.5772/intechopen.1001513. Available from: (PDF) Beta Cell Regulation, Function, Dysfunction and Eventual Destruction in Type 1 Diabetes. Last accessed on May 26, 2025.
- Giwa AM, Ahmed R, Omidian Z, et al. Current understandings of the pathogenesis of type 1 diabetes: Genetics to environment. World J Diabetes. 2020;11(1):13-25. doi:10.4239/wjd.v11.i1.13.
- Barker JM. Clinical review: Type 1 diabetes-associated autoimmunity: natural history, genetic associations, and screening. J Clin Endocrinol Metab. 2006;91(4):1210-1217. doi:10.1210/jc.2005-1679.
- Lizzo JM, Goyal A, Gupta V. Adult Diabetic Ketoacidosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; July 10, 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560723/. Last accessed on May 26, 2025.
- Sims EK, Besser REJ, Dayan C, et al. Screening for Type 1 Diabetes in the General Population: A Status Report and Perspective. Diabetes. 2022;71(4):610-623. doi:10.2337/dbi20-0054.
- Haller MJ, Bell KJ, Besser REJ, et al. ISPAD Clinical Practice Consensus Guidelines 2024: Screening, Staging, and Strategies to Preserve Beta-Cell Function in Children and Adolescents with Type 1 Diabetes. Horm Res Paediatr. 2024;97(6):529-545. doi:10.1159/000543035.
- Stages of type 1 diabetes & why they’re important | JDRF Australia. Available at: https://breakthrought1d.org.au/what-is-t1d/stages/. Last accessed on May 26, 2025.
- Al-Mulla F, Alhomaidah D, Abu-Farha M, et al. Early autoantibody screening for type 1 diabetes: a Kuwaiti perspective on the advantages of multiplexing chemiluminescent assays. Front Immunol. 2023;14:1273476. doi:10.3389/fimmu.2023.1273476.
- Moore DJ, Leibel NI, Polonsky W, Rodriguez H. Recommendations for Screening and Monitoring the Stages of Type 1 Diabetes in the Immune Therapy Era. Int J Gen Med. 2024;17:3003-3014. doi:10.2147/IJGM.S438009.
MAT-GLB-2502136-1.0-05/2025