- Article
- Source: Campus Sanofi
- Nov 10, 2025
Improving Quality of Life in Patients with Uncontrolled Atopic Dermatitis (AD): Tools for Timely Identification and Treatment

Introduction
Atopic dermatitis (AD), a chronic inflammatory skin condition, poses significant challenges in pediatric, adolescent and adult patients.1 A key factor in the pathophysiology of AD is the underlying type 2 inflammation, driven by cytokines such as IL-4 and IL-13. 2,3 This type 2 inflammation can contribute to barrier dysfunction, intense itch and increased risk of skin infections.2,3 The impact of moderate-to-severe AD is multifaceted, and the long-term risks of uncontrolled AD may extend beyond visible skin symptoms.4,5
Understanding the Burden Beyond Skin Symptoms
The symptoms of AD can affect not only the skin but also the overall quality of life, including social, emotional, and physical health. The combined effect of these factors, over time, in uncontrolled AD can lead to a cumulative life course impairment (CLCI) for some patients. 4-7 Recognizing these broader implications is essential for an effective management.6
A range of tools have been developed to help identify those patients whose AD remains uncontrolled despite current therapy. 6,8
Tools for Identifying Uncontrolled Atopic Dermatitis
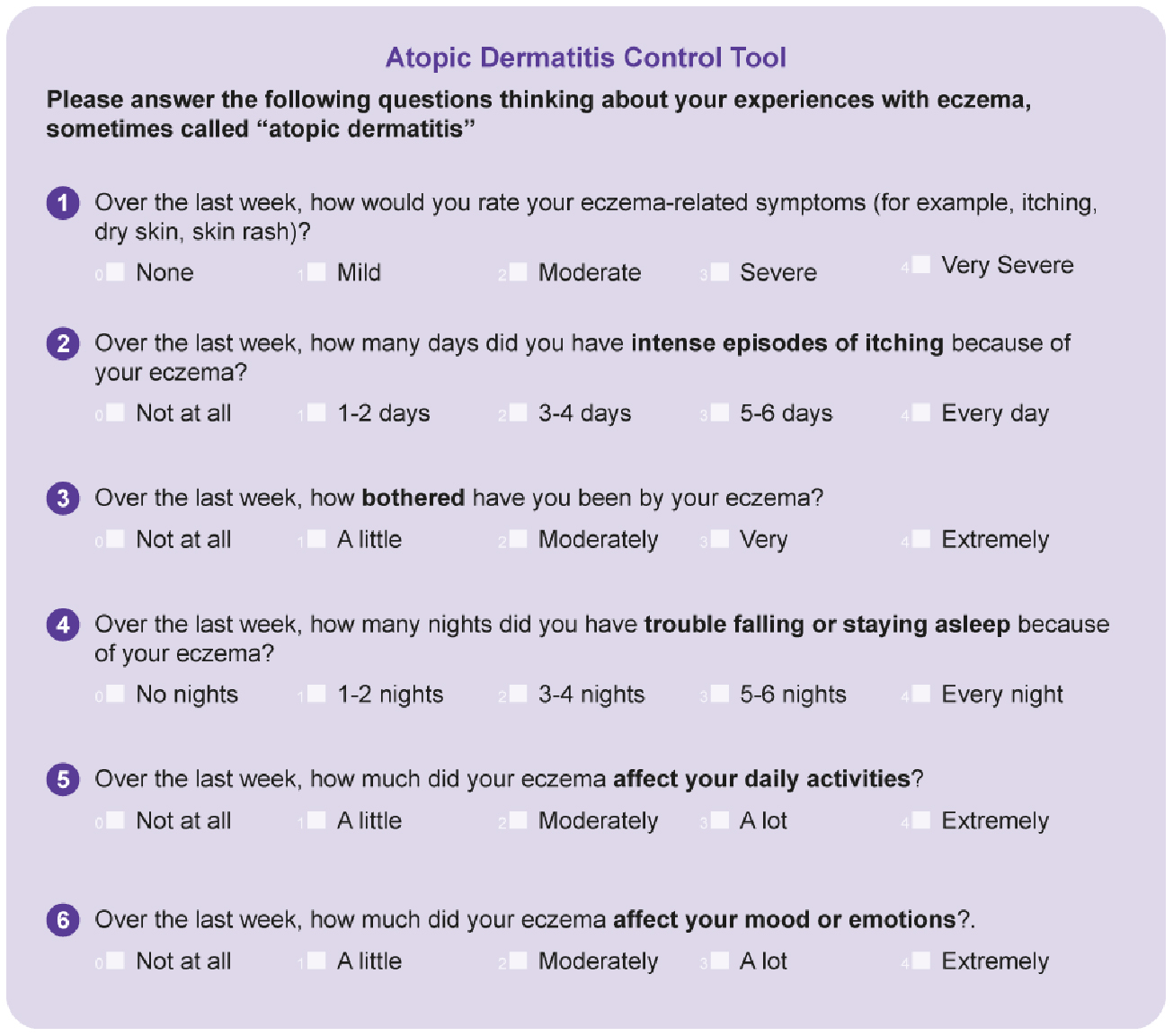
The Atopic Dermatitis Control Tool (ADCT) provide valuable insights into evaluating the extent of the condition and guiding healthcare providers to make informed treatment decisions. 9,10
Atopic Dermatitis Control Tool (ADCT): This tool is designed to facilitate meaningful discussions between patients and healthcare providers regarding the control of AD in clinical practice. This validated tool is appropriate for patients 12 years and older and it consists of six questions that evaluate the severity of symptoms, including itch and sleep disturbances, and their impact on daily activities and mood. Within a range of 0 to 24, a score of ≥7 indicates inadequate disease control, which prompts a reassessment of treatment strategies. The ACDT helps in identifying the degree of disease control and making informed decisions about escalating therapy.9,10
.jpg)
Please Click here to access the ADCT – a validated, brief and easily scored patient self- assessment tool.
Potential Future Tools for Assessing Cumulative Life Course Impairment
Tools to address the CLCI caused by AD will be essential for understanding and managing the profound impacts of AD throughout patients’ lives. Recent developments in this area show promise, though it's important to note these tools are still in development stages.8
.jpg)
Dermatology CLCI Retrospective (DermCLCI-r) tool
Aims to assess the CLCI caused by AD, focusing on how the disease has affected patients’ lives over time. It includes questions on physical, emotional, and social domains, offering a comprehensive view of past impacts.8
.jpg)
Dermatology CLCI prospective (DermCLCI-p) tool
Conversely, the DermCLCI-p tool is intended to predict future risks associated with AD, helping to identify patients at risk for life impairment.8
Both tools consist of 30-item questionnaire that helps assess the impairments of AD. This questionnaire assesses the following:8
- The effect of life course impairment on a 4-point Likert scale [0 (not at all) to 3 (very)] and whether these have been life-changing
- The effect of coping behaviors on a 5-point Likert scale [0 (not at all) to 4 (very)]
These tools are still in their early stages and await comprehensive psychometric testing for validity and reliability. Development of these tools is an important first step in better understanding the experience of disease burden within the context of additional impactful life events. With future study, they hold promise for integration into both routine clinical care and broader health services research.8
When AD is refractory to topical therapies, advanced treatment with phototherapy or systemic medications can be considered. Advanced systemic therapies, including biologics or Janus kinase inhibitors (JAKis), may be effective in treating moderate-to-severe AD.11-14
Conclusion
Understanding and using these tools can contribute to a better management of AD. 10 By recognizing the extensive burden of AD beyond the skin, clinicians are better equipped to identify patients who are not well controlled on their current medications. This awareness may better inform decisions about when treatment escalation may be required to address both immediate symptoms and long-term impact on the patient’s quality of life.8,10
- Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109-1122. doi:10.1016/S0140-6736(15)00149-X
- Haddad EB, Cyr SL, Arima K, McDonald RA, Levit NA, Nestle FO. Current and Emerging Strategies to Inhibit Type 2 Inflammation in Atopic Dermatitis. Dermatol Ther (Heidelb). 2022;12(7):1501-1533. doi:10.1007/s13555-022-00737-7
- Moniaga CS, Tominaga M, Takamori K. The Pathology of Type 2 Inflammation-Associated Itch in Atopic Dermatitis. Diagnostics. 2021; 11(11):2090. doi:10.3390/diagnostics11112090
- Fasseeh AN, Elezbawy B, Korra N, et al. Burden of Atopic Dermatitis in Adults and Adolescents: a Systematic Literature Review. Dermatol Ther (Heidelb). 2022;12(12):2653-2668. doi:10.1007/s13555-022-00819-6
- Weidinger S, Simpson EL, Silverberg JI, et al. Burden of atopic dermatitis in paediatric patients: an international cross-sectional study. Br J Dermatol. 2024;190(6):846-857. doi:10.1093/bjd/ljad449.
- Calzavara-Pinton P, Čelakovská J, Lapeere H, et al. Baseline Demographics, Comorbidities, Treatment Patterns and Burden of Atopic Dermatitis in Adults and Adolescents from the GLOBOSTAD Long-Term Observational Study. Adv Ther. 2023;40(12):5366-5382. doi:10.1007/s12325-023-02644-5.
- Kimball AB, Gieler U, Linder D, Sampogna F, Warren RB, Augustin M. Psoriasis: is the impairment to a patient's life cumulative?. J Eur Acad Dermatol Venereol. 2010;24(9):989 1004. doi:10.1111/j.1468-3083.2010.03705.x
- Braren-von Stülpnagel CC, Augustin M, Westphal L, Sommer R. Development of Measurement Tools to Assess Cumulative Life Course Impairment in Patients with Chronic Skin Diseases. J Eur Acad Dermatol Venereol. Published online February 18, 2023. doi:10.1111/jdv.18977
- Strober B, Mallya UG, Yang M, et al. Treatment Outcomes Associated With Dupilumab Use in Patients With Atopic Dermatitis: 1-Year Results From the RELIEVE-AD Study. JAMA Dermatol. 2022;158(2):142-150. doi:10.1001/jamadermatol.2021.4778
- ADCT, Atopic Dermatitis Control Tool. Patient Form. Accessed May 14, 2025. https://www.adcontroltool.com/adct-downloads1
- Chovatiya R, Silverberg JI. Evaluating the Longitudinal Course of Atopic Dermatitis: Implications for Clinical Practice. Am J Clin Dermatol. 2022;23(4):459-468. doi:10.1007/s40257-022-00697-w
- Davis DMR, Drucker AM, Alikhan A, et al. Guidelines of care for the management of atopic dermatitis in adults with phototherapy and systemic therapies. J Am Acad Dermatol. 2024;90(2):e43-e56. doi:10.1016/j.jaad.2023.08.102
- AAAAI/ACAAI JTF Atopic Dermatitis Guideline Panel, Chu DK, Schneider L, et al. Atopic dermatitis (eczema) guidelines: 2023 American Academy of Allergy, Asthma and Immunology/American College of Allergy, Asthma and Immunology Joint Task Force on Practice Parameters GRADE- and Institute of Medicine-based recommendations. Ann Allergy Asthma Immunol. 2024;132(3):274-312. doi:10.1016/j.anai.2023.11.009
- Chu AWL, Wong MM, Rayner DG, et al. Systemic treatments for atopic dermatitis (eczema): Systematic review and network meta-analysis of randomized trials. J Allergy Clin Immunol. 2023;152(6):1470-1492. doi:10.1016/j.jaci.2023.08.029
MAT-BH-2500560/V1/November 2025