- Article
- Source: Campus Sanofi
- Nov 10, 2025
The Hidden Impact of Cumulative Life Course Impairment (CLCI) in Dermatology: An Overview

Introduction
Skin diseases are the fourth most common cause of nonfatal morbidity, impacting nearly one-third of the global population. Chronic diseases cause substantial burden, and despite their high prevalence, this burden is often underestimated.1,2
Chronic skin diseases including atopic dermatitis (AD), psoriasis, and hidradenitis suppurativa (HS), notably affect patients' health-related quality of life (HRQoL), including physical health, emotional well-being, and social interactions. Patients with inflammatory skin diseases often suffer from symptoms that contribute to psychological distress, including anxiety and depression, ultimately resulting in cumulative long-term impairment.3 Understanding Cumulative Life Course Impairment (CLCI) is essential to fully grasp the enduring burden of chronic skin diseases and the irreversible impact on patients' lives over time.4
This article will further discuss the concept of CLCI in dermatology, explore the chronic nature of AD and its impact on patients.
CLCI in Dermatology: What You Need to Know?
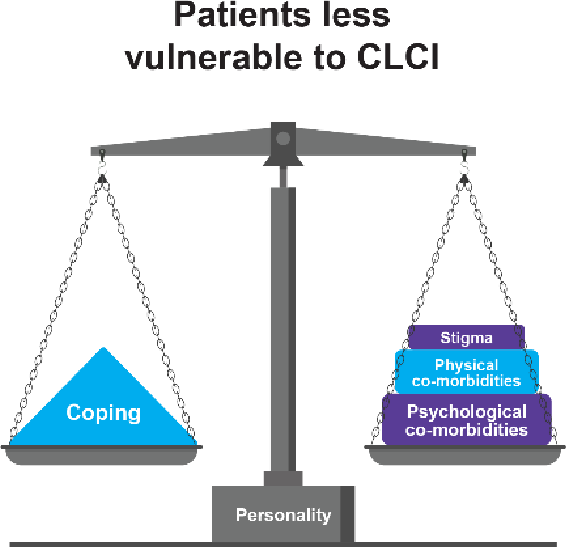
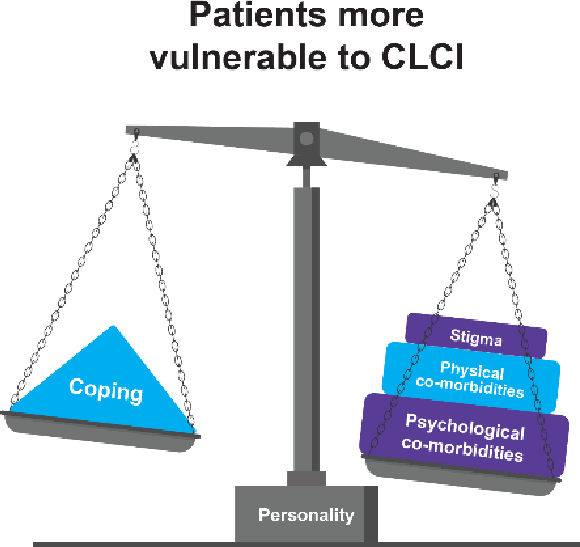
Cumulative Life Course Impairment (CLCI) is a theoretical concept that describes the non- reversible burden of chronic skin diseases over time. In some cases, this persistent burden can lead to chronic impairment and missed opportunities resulting in lasting psychosocial and personal damage. Some individuals are less vulnerable to CLCI, while others are more affected by factors such as stigma, physical comorbidities, and psychological comorbidities. Difficulty in coping with these factors increases the patients' risk of vulnerability.4
Hypothetical impairment over a patient’s life course4
Recognizing these factors is crucial for healthcare professionals to develop comprehensive management strategies aimed at mitigating the long-term effects of chronic skin diseases such as AD.
The Chronic Nature of AD: A Multidimensional Burden
Atopic dermatitis (AD) is a chronic, relapsing condition marked by eczematous lesions and severe pruritus. Although AD often manifests in infancy, affecting approximately 20% of children, it remains highly prevalent in adults, indicating a lifelong disposition.5
The chronic nature of AD can lead to a continuous cycle of flare-ups and remissions. The atopic comorbidities such as food allergies, asthma, allergic rhinitis, other immune-mediated inflammatory diseases, and non-atopic comorbidities such as metabolic syndrome, cardiovascular complications, osteoporosis, mental health disorders, etc., may develop in patients with severe disease4-6
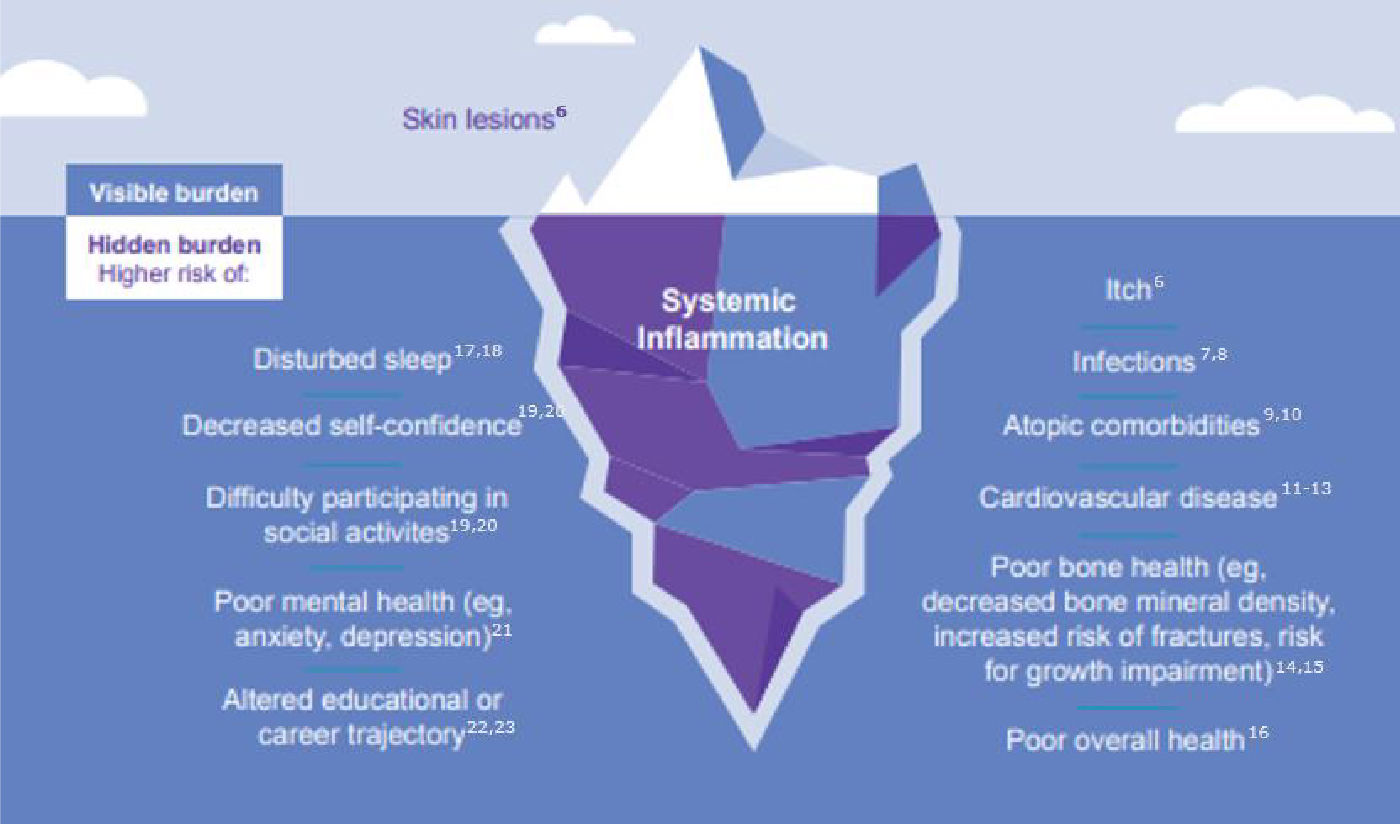
The burden of uncontrolled AD may further lead to other factors such as sleep loss, impaired functioning, self-esteem issues, reduced productivity, cardiovascular diseases, poor bone health, financial strain, and loss of opportunities.23-27
High Disease Burden in Low BSA Involvement
This chronic and relapsing nature of AD underscores the importance of evaluating the disease's impact, even when the Body Surface Area (BSA) involvement is minimal.
Patients with a BSA involvement may experience a high disease burden. 28 The severity of symptoms and their impact on QoL are not solely dependent on the extent of skin involvement but also on the functionality and visibility of the affected areas. 28,29
Hands and feet constitute ≈8% of BSA affected by AD, and face constitutes ≈4.5% (according to the rule of nines). These areas can lead to significant physical impairments that affect the QoL, causing psychological distress and disrupting work and school productivity.29-34
Over time, these ongoing challenges can contribute to CLCI, highlighting the long-term, cumulative burden of chronic skin diseases.3
Timely intervention and escalation of therapy for patients with uncontrolled moderate to severe AD can be critical in helping to manage the signs, symptoms and quality of life impacts of uncontrolled AD. 27
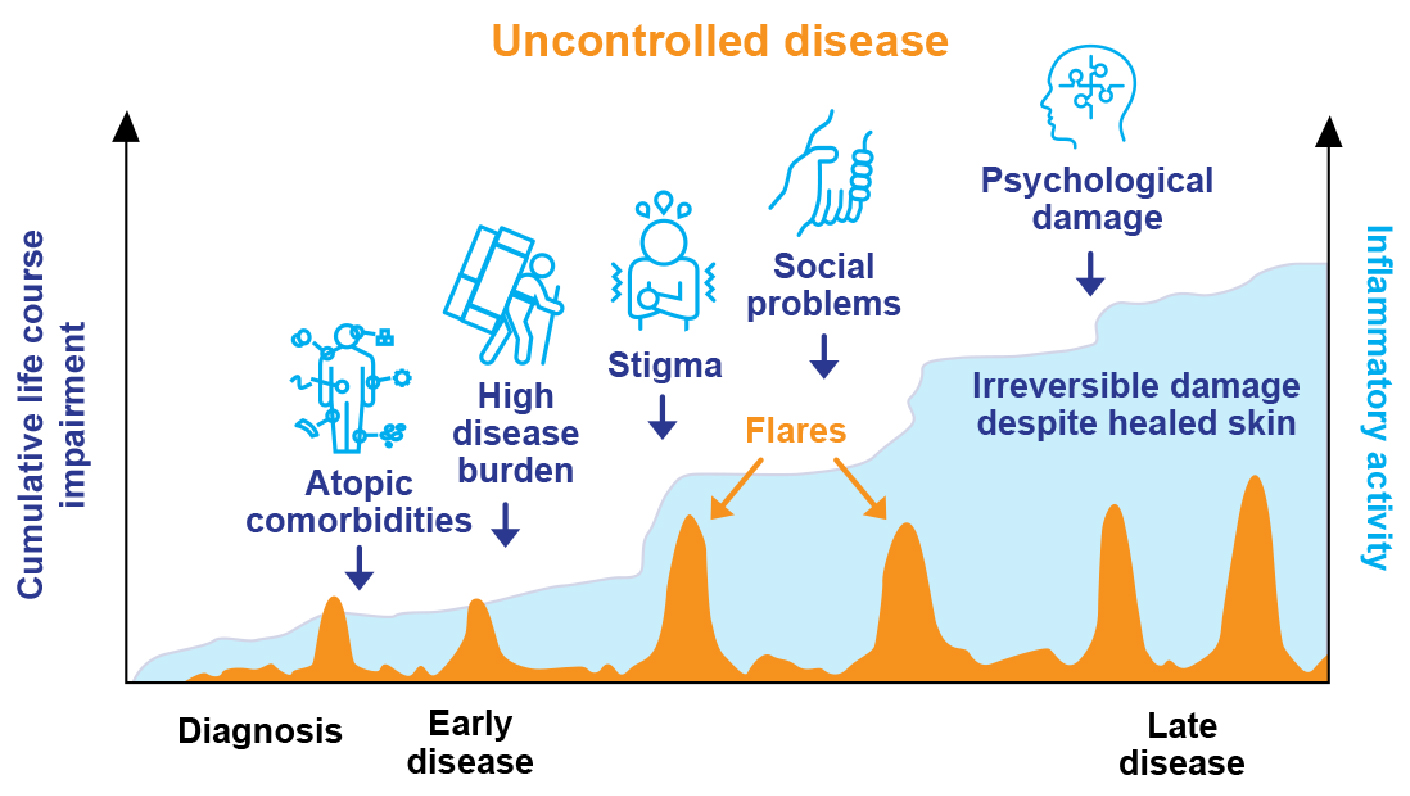
The graph is a model of CLCI throughout the course of AD, adapted from
Kimball, et al. J Eur Acad Dermatol Venereol. 201027 and Bieber T, et al. Nat Rev Drug Discov. 2023.35
Conclusion
Cumulative Life Course Impairment (CLCI) is a crucial concept in understanding the long-term impact of chronic skin conditions like AD. 3,4
For patients with moderate-to-severe AD, the burden extends beyond the skin, causing psychological and social distress, and affecting the overall QoL.29-31
Timely and appropriate escalation for patients suffering with uncontrolled AD may help reduce the burdens they face.36
CTA:
Cumulative Life Course Impairment in AD: Beyond Skin Symptoms
- Seth D, Cheldize K, Brown D, Freeman EF. Global Burden of Skin Disease: Inequities and Innovations. Curr Dermatol Rep. 2017 Sep;6(3):204-210. doi:10.1007/s13671-017- 0192-7.
- Flohr C, Hay R. Putting the burden of skin diseases on the global map. Br J Dermatol. 2021;184:189-190. doi:https://doi.org/10.1111/bjd.19704.
- von Stülpnagel CC, Augustin M, Düpmann L, da Silva N, Sommer R. Mapping risk factors for cumulative life course impairment in patients with chronic skin diseases - a systematic review. J Eur Acad Dermatol Venereol. 2021;35(11):2166-2184. doi:10.1111/jdv.17348.
- Augustin A, Mayer A, Goepel LM, Baade K, Heyer K, Herberger K. Cumulative Life Course Impairment (CLCI): A new concept to characterize persistent patient burden in chronic wounds. Wound Medicine. 2013;1:2-6. doi: https://doi.org/10.1016/j.wndm.2013.06.001.
- Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109-1122. doi:10.1016/S0140-6736(15)00149-X.
- Simpson EL, Bieber T, Eckert L, Wu R, Ardeleanu M, Graham NM, Pirozzi G, Mastey V. Patient burden of moderate to severe atopic dermatitis (AD): Insights from a phase 2b clinical trial of dupilumab in adults. J Am Acad Dermatol. 2016;74(3):491-8. doi:10.1016/j.jaad.2015.10.043.
- Wang V, Boguniewicz J, Boguniewicz M, Ong PY. The infectious complications of atopic dermatitis. Ann Allergy Asthma Immunol. 2021;126(1):3-12. doi:10.1016/j.anai.2020.08.002.
- Cameron S, Donnelly A, Broderick C, et al. Mind and skin: Exploring the links between inflammation, sleep disturbance and neurocognitive function in patients with atopic dermatitis. Allergy. 2024;79(1):26-36. doi:10.1111/all.15818.
- Weidinger S, Simpson EL, Silverberg JI, et al. Burden of atopic dermatitis in paediatric patients: an international cross-sectional study. Br J Dermatol. 2024;190(6):846-857. doi:10.1093/bjd/ljad449
- Calzavara-Pinton P, Čelakovská J, Lapeere H, et al. Baseline Demographics, Comorbidities, Treatment Patterns and Burden of Atopic Dermatitis in Adults and Adolescents from the GLOBOSTAD Long-Term Observational Study. Adv Ther. 2023;40(12):5366-5382. doi:10.1007/s12325-023-02644-5.
- Lee SW, Kim H, Byun Y, et al. Incidence of Cardiovascular Disease After Atopic Dermatitis Development: A Nationwide, Population-Based Study. Allergy Asthma Immunol Res. 2023;15(2):231-245. doi:10.4168/aair.2023.15.2.231.
- Lundin S, Wahlgren CF, Johansson EK, et al. Childhood atopic dermatitis is associated with cardiovascular risk factors in young adulthood-A population-based cohort study. J Eur Acad Dermatol Venereol. 2023;37(9):1854-1862. doi:10.1111/jdv.19190.
- Wan J, Fuxench ZCC, Wang S, et al. Incidence of Cardiovascular Disease and Venous Thromboembolism in Patients With Atopic Dermatitis. J Allergy Clin Immunol Pract. 2023;11(10):3123-3132.e3. doi:10.1016/j.jaip.2023.08.007.
- Silverberg JI, Paller AS. Association between eczema and stature in 9 US population- based studies. JAMA Dermatol. 2015;151(4):401-409. doi:10.1001/jamadermatol.2014.3432.
- Wu D, Wu XD, Zhou X, Huang W, Luo C, Liu Y. Bone mineral density, osteopenia, osteoporosis, and fracture risk in patients with atopic dermatitis: a systematic review and meta-analysis. Ann Transl Med. 2021;9(1):40. doi:10.21037/atm-20-4708.
- Silverberg JI, Garg NK, Paller AS, Fishbein AB, Zee PC. Sleep Disturbances in Adults with Eczema Are Associated with Impaired Overall Health: A US Population-Based Study. J Invest Dermatol. 2015;135:56–66. doi: 10.1038/jid.2014.325.
- Chang YS, Chiang BL. Sleep disorders and atopic dermatitis: A 2-way street?. J Allergy Clin Immunol. 2018;142(4):1033-1040. doi:10.1016/j.jaci.2018.08.005.
- Paller AS, Guttman-Yassky E, Schuttelaar MLA, et al. Disease characteristics, comorbidities, treatment patterns and quality of life impact in children <12 years old with atopic dermatitis: Interim results from the PEDISTAD Real-World Registry. J Am Acad Dermatol. 2022;87(5):1104-1108. doi:10.1016/j.jaad.2022.01.018.
- Paller AS, Weidinger S, Capozza K, et al. Similarities and Differences in the Perception of Atopic Dermatitis Burden Between Patients, Caregivers, and Independent Physicians (AD-GAP Survey). Dermatol Ther (Heidelb). 2023;13(4):961-980. doi:10.1007/s13555- 022-00850-7.
- Neri I, Galli E, Baiardini I, et al. Implications of Atopic Dermatitis on the Quality of Life of 6-11 Years Old Children and Caregivers (PEDI-BURDEN). J Asthma Allergy. 2023;16:383-396. Published 2023 Apr 12. doi:10.2147/JAA.S404350.
- Girolomoni G, Luger T, Nosbaum A, et al. The Economic and Psychosocial Comorbidity Burden Among Adults with Moderate-to-Severe Atopic Dermatitis in Europe: Analysis of a Cross Sectional Survey. Dermatol Ther (Heidelb). 2021;11(1):117-130. doi:10.1007/s13555-020-00459-8.
- Ibler K, Jemec GB. Cumulative life damage in dermatology. Dermatol Reports. 2011 Apr 12;3(1):e5. doi: 10.4081/dr.2011.e5.
- Bacci ED, Correll JR, Pierce EJ, et al. Burden of adult atopic dermatitis and unmet needs with existing therapies. J Dermatolog Treat. 2023;34(1):2202288. doi:10.1080/09546634.2023.2202288.
- Fasseeh AN, Elezbawy B, Korra N, et al. Burden of Atopic Dermatitis in Adults and Adolescents: a Systematic Literature Review. Dermatol Ther (Heidelb). 2022;12(12):2653-2668. doi:10.1007/s13555-022-00819-6.
- Davis DMR, Drucker AM, Alikhan A, et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86(6):1335-1336.e18. doi:10.1016/j.jaad.2022.01.009.
- Thyssen JP, Halling AS, Schmid-Grendelmeier P, Guttman-Yassky E, Silverberg JI. Comorbidities of atopic dermatitis-what does the evidence say?. J Allergy Clin Immunol. 2023;151(5):1155-1162. doi:10.1016/j.jaci.2022.12.002.
- Kimball AB, Gieler U, Linder D, Sampogna F, Warren RB, Augustin M. Psoriasis: is the impairment to a patient's life cumulative?. J Eur Acad Dermatol Venereol. 2010;24(9):989-1004. doi:10.1111/j.1468-3083.2010.03705.x.
- Silverberg JI, Mohawk JA, Cirulli J, et al. Burden of Disease and Unmet Needs in Atopic Dermatitis: Results From a Patient Survey. Dermatitis. 2023;34(2):135-144. doi:10.1089/derm.2022.29015.jsi
- Simpson EL, Silverberg JI, Worm M, et al. Dupilumab treatment improves signs, symptoms, quality of life, and work productivity in patients with atopic hand and foot dermatitis: Results from a phase 3, randomized, double-blind, placebo-controlled trial. J Am Acad Dermatol. 2024;90(6):1190-1199. doi:10.1016/j.jaad.2023.12.066.
- Grant L, Seiding Larsen L, Burrows K, et al. Development of a Conceptual Model of Chronic Hand Eczema (CHE) Based on Qualitative Interviews with Patients and Expert Dermatologists. Adv Ther. 2020;37(2):692-706. doi:10.1007/s12325-019-01164-5
- Silverberg JI, Simpson B, Abuabara K, et al. Prevalence and burden of atopic dermatitis involving the head, neck, face, and hand: A cross sectional study from the TARGET- DERM AD cohort. J Am Acad Dermatol. 2023;89(3):519-528. doi:10.1016/j.jaad.2023.04.052.
- Jaros J, Hendricks AJ, Shi VY, Lio PA. A Practical Approach to Recalcitrant Face and Neck Dermatitis in Atopic Dermatitis. Dermatitis. 2020;31(3):169-177. doi:10.1097/DER.0000000000000590.
- Rønnstad ATM, Thomsen SF, Thyssen JP, Egeberg A. The burden of head-and-neck dermatitis in adults with atopic dermatitis and its association with asthma, rhinitis, and disease severity. J Am Acad Dermatol. 2024;90:616–618. doi:10.1016/j.jaad.2023.10.042.
- Moore RA, Popowicz P, Burns B. Rule of Nines. [Updated 2024 Feb 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-Available from: https://www.ncbi.nlm.nih.gov/books/NBK513287/
- Bieber T. Disease modification in inflammatory skin disorders: opportunities and challenges [published correction appears in Nat Rev Drug Discov. 2023 Nov;22(11):935. doi: 10.1038/s41573-023-00790-7.]. Nat Rev Drug Discov. 2023;22(8):662-680. doi:10.1038/s41573-023-00735-0.
- Davis DMR, Drucker AM, Alikhan A, et al. Guidelines of care for the management of atopic dermatitis in adults with phototherapy and systemic therapies. J Am Acad Dermatol. 2024;90(2):e43-e56. doi:10.1016/j.jaad.2023.08.102.
MAT-BH-2500558/V1/November 2025