- Article
- Source: Campus Sanofi
- Nov 10, 2025
Unseen Burdens: How Cumulative Life Course Impairment (CLCI) Affects Patients with Moderate-to-Severe Atopic Dermatitis (AD)

Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin condition characterized by intense itching and periodic flares of inflamed, dry skin which may eventually impair patients' quality of life (QoL).1,2 The underlying pathophysiology of AD involves type 2 inflammation (T2I), driven by cytokines such as interleukin (IL)-4 and IL-13, which exacerbate symptoms and contribute to the disease's complexity.3 However, the burden of uncontrolled moderate-to-severe AD can extend far beyond the visible symptoms, encompassing psychological and social impact that contribute to Cumulative Life Course Impairment (CLCI).2,4
According to the Global Burden of Disease study, AD has the highest disability-adjusted life-year (DALY) burden among all skin diseases, with an age-standardized DALY rate significantly higher than psoriasis and urticaria.2
This article focuses on understanding CLCI in AD, and the importance of recognizing and addressing these hidden burdens.
Moderate-to-Severe Atopic Dermatitis–A Cumulative Burden
The multidimensional burdens of AD in patients with moderate-to-severe symptoms affect more than just skin lesions and itching.1,5,6 Patients frequently suffer from specific elements of CLCI such as stigma, psychological distress, limited social support, and coping challenges, all of which contribute to CLCI.4
Stigma
Patients with AD often face social stigma due to overt public rejection, self-image, and lack of self-confidence4
Psychological Burden
Psychological comorbidities of people living with AD include anxiety, depression, suicidal ideation, alexithymia, and addiction—further complicating the patient's health profile4
Systemic Implications
The chronic inflammation can lead to comorbidities such as poor bone health, cardiovascular diseases, metabolic syndrome (hypertension, diabetes, obesity), and other immune-related conditions4
Social Support
Additionally, the lack of adequate social support from family, friends, colleagues can hinder effective management of the disease, leading to a sense of isolation and helplessness among patients4
Coping Challenges
Maladptive coping, mental disagreement, denial, helplessness and family factors add to coping challenges.These challenges add to the cumulative burden, making it difficult for patients to maintain a normal lifestyle4
The cumulative effect of these burdens over the years can lead to a potentially irreversible damage, affecting various life domains such as productivity at school and work, and the ability to maintain social relationships.2,4,7
CLCI–Potentially Irreversible Damage Due to Inadequate Treatment and Uncontrolled AD
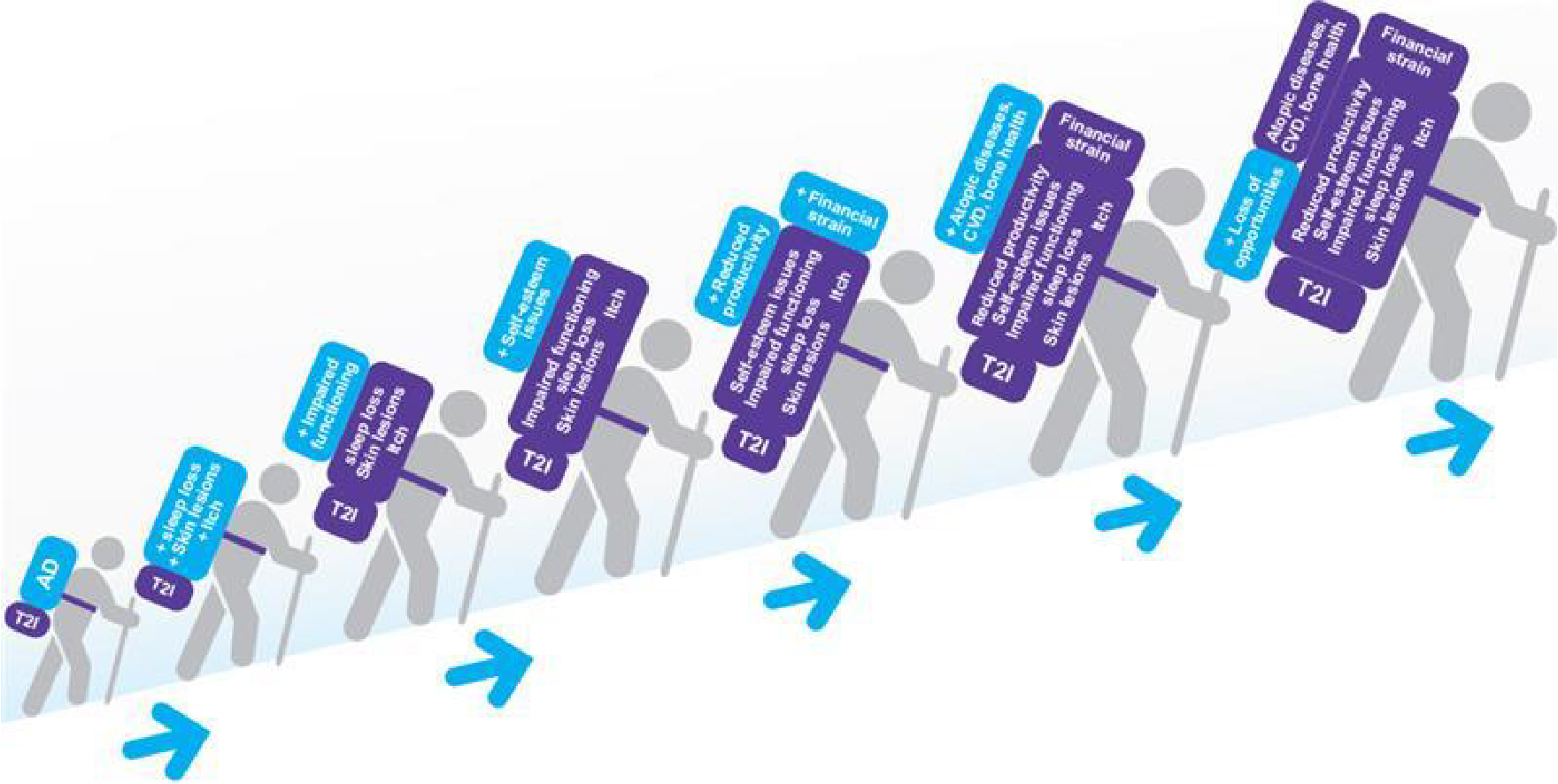
Timely identification and treatment escalation of patients with uncontrolled AD may improve the signs, symptoms and quality of life burdens these patients are currently experiencing. 7
Conclusion
The burdens of uncontrolled AD may become cumulative, impacting various aspects of a patient's life and contributing to CLCI. 1,4,6 By understanding and addressing these multifaceted challenges, healthcare professionals can improve patient outcomes and quality of life.2,7 Early identification of at-risk patients, using appropriate tools, and timely escalation to appropriate treatments are crucial in providing best practice care for patients. 4,7,11
- Weidinger S, Novak N. Atopic dermatitis. Lancet. 2016;387(10023):1109-1122. doi:10.1016/S0140-6736(15)00149-X.
- Fasseeh AN, Elezbawy B, Korra N, et al. Burden of Atopic Dermatitis in Adults and Adolescents: a Systematic Literature Review. Dermatol Ther (Heidelb). 2022;12(12):2653-2668. doi:10.1007/s13555-022-00819-6.
- Moniaga CS, Tominaga M, Takamori K. The Pathology of Type 2 Inflammation-Associated Itch in Atopic Dermatitis. Diagnostics (Basel). 2021;11(11):2090. Published 2021 Nov 12. doi:10.3390/diagnostics11112090.
- Kimball AB, Gieler U, Linder D, Sampogna F, Warren RB, Augustin M. Psoriasis: is the impairment to a patient's life cumulative?. J Eur Acad Dermatol Venereol. 2010;24(9):989 1004. doi:10.1111/j.1468-3083.2010.03705.x.
- Weidinger S, Simpson EL, Silverberg JI, et al. Burden of atopic dermatitis in paediatric patients: an international cross-sectional study. Br J Dermatol. 2024;190(6):846-857. doi:10.1093/bjd/ljad449.
- Calzavara-Pinton P, Čelakovská J, Lapeere H, et al. Baseline Demographics, Comorbidities, Treatment Patterns and Burden of Atopic Dermatitis in Adults and Adolescents from the GLOBOSTAD Long-Term Observational Study. Adv Ther. 2023;40(12):5366-5382. doi:10.1007/s12325-023-02644-5.
- von Stülpnagel CC, Augustin M, Düpmann L, da Silva N, Sommer R. Mapping risk factors for cumulative life course impairment in patients with chronic skin diseases - a systematic review. J Eur Acad Dermatol Venereol. 2021;35(11):2166-2184. doi:10.1111/jdv.17348.
- Davis DMR, Drucker AM, Alikhan A, et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J Am Acad Dermatol. 2022;86(6):1335-1336.e18. doi:10.1016/j.jaad.2022.01.009.
- Thyssen JP, Halling AS, Schmid-Grendelmeier P, Guttman-Yassky E, Silverberg JI. Comorbidities of atopic dermatitis-what does the evidence say?. J Allergy Clin Immunol. 2023;151(5):1155-1162. doi:10.1016/j.jaci.2022.12.002.
- Bacci ED, Correll JR, Pierce EJ, et al. Burden of adult atopic dermatitis and unmet needs with existing therapies. J Dermatolog Treat. 2023;34(1):2202288. doi:10.1080/09546634.2023.2202288.
- Bieber T. Disease modification in inflammatory skin disorders: opportunities and challenges [published correction appears in Nat Rev Drug Discov. 2023 Nov;22(11):935. doi: 10.1038/s41573-023-00790-7.]. Nat Rev Drug Discov. 2023;22(8):662-680. doi:10.1038/s41573- 023-00735-0.
MAT-BH-2500559/V1/November 2025