- Article
- Source: Campus Sanofi
- 27 Jan 2025
Key tools to measure the success of COPD management

This article provides respiratory physicians with essential insights into evaluating COPD management. It delves into the multifaceted approach required to measure success, including reducing symptom severity, preventing exacerbations, improving lung function, enhancing exercise tolerance, and help boosting the quality of life.1,2 By employing standardised assessment tools such as the COPD Assessment Test (CAT), modified Medical Research Council (mMRC) dyspnea scale, and St. George’s Respiratory Questionnaire (SGRQ), clinicians can accurately gauge treatment effectiveness.3-7 Additionally, the article highlights the importance of continuous assessment and adjustment in managing COPD, helping to ensure better patient outcomes.1-7
Learn more on how to assess these goals below
How to evaluate success in achieving treatment goals?
Success in managing chronic obstructive pulmonary disease (COPD) is multifaceted and can be measured by reduction in symptom severity and disease progression, clinically meaningful reductions in exacerbations, significant improvement in lung function, improved exercise tolerance and an increase in a patient’s quality of life (QoL).1,2 Treatment success requires a continuous cycle of assessment, treatment adjustment, and a review of response. Evidence-based metrics can be used to gauge outcomes in COPD patients and provide a structured way to assess the effectiveness of treatments and guide clinical decisions towards improving the lives of patients with COPD as discussed in the following sections.1,2
What is the impact of exacerbations on patients’ disease trajectory?
Frequent exacerbations are associated with poor health status, morbidity, and mortality.8 They can result in a decline in lung function and frequent hospitalisations. Minimising the negative impact of ongoing exacerbations and reducing the number and severity of exacerbations is critical to COPD management.1,8
To learn more about the impact of exacerbations, read this article The Impact of exacerbations in COPD | Campus Sanofi.
How is lung function assessed in patients with COPD?
Rapidly declining lung function in patients with COPD results in impaired health status and increased risk of mortality.9 Assessment of lung function by spirometry, particularly the Forced Expiratory Volume in 1 second9 (FEV1), plays an important role in determining the severity of COPD and guiding treatment.1,9 A slower decline in FEV1 over time is indicative of successful disease management.
How can symptoms and their impact be assessed?
Symptoms impact the daily lives of patients by significantly influencing physical activity, health status and QoL.2 COPD treatment guidelines recommend using standardised multidimensional measures, COPD Assessment Test (CAT), modified Medical Research Council (mMRC) Dyspnea Scale and, St. George’s Respiratory Questionnaire (SGRQ), for assessing health status and QoL.1-7
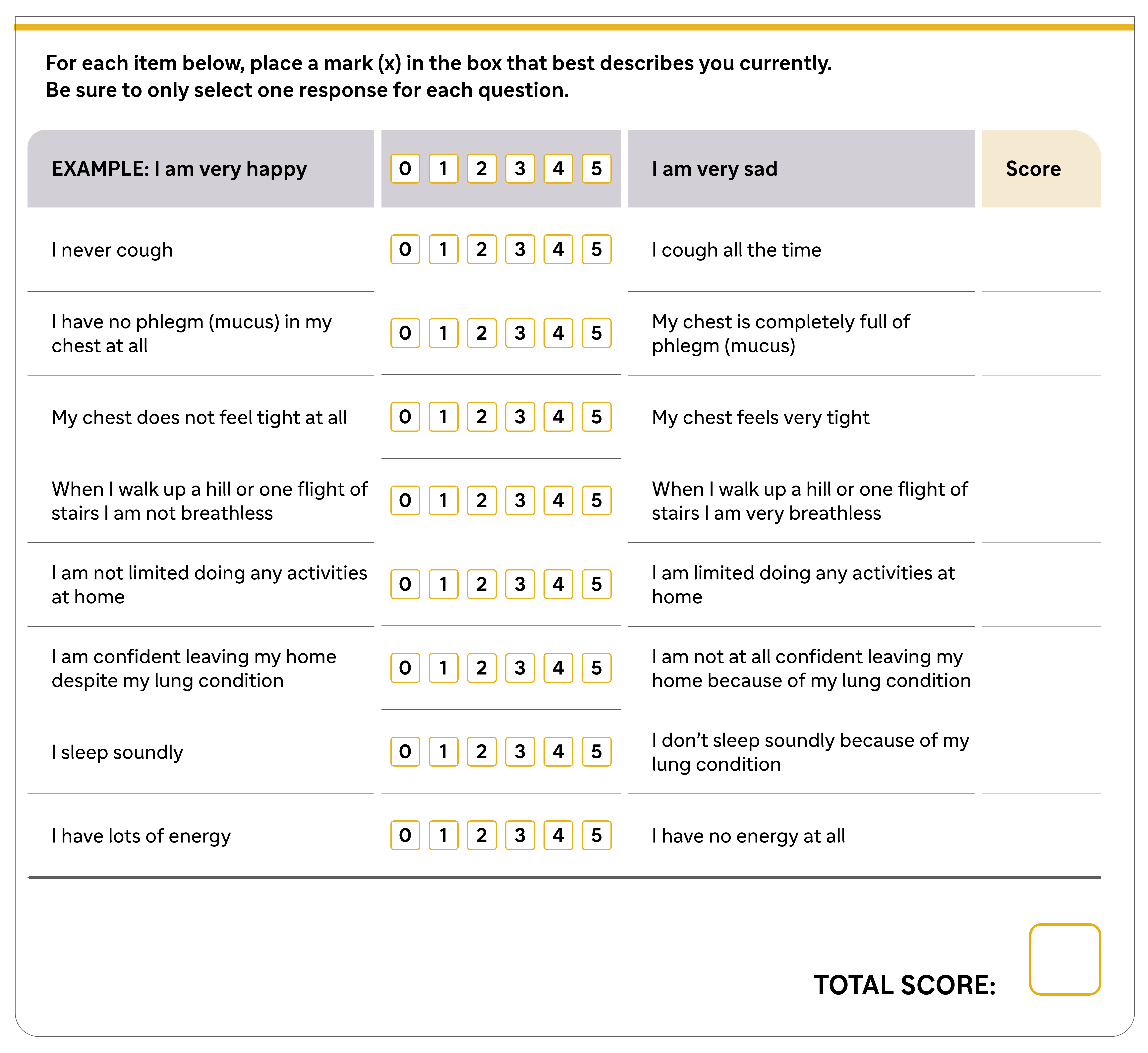
Which symptoms can be scored on CAT?
CAT is a questionnaire that assesses and scores 8 functional parameters — cough, phlegm, chest tightness, breathlessness while climbing up a hill or flight of stairs, activity limitation at home, confidence leaving home, sleep, and energy. These 8 parameters are scored on a scale of 0 to 5, with a total score of 40.1-4 The CAT score provides a measure of the impact of disease on patient’s daily life. A CAT score of 5 is the upper limit of normal in healthy non-smoking individuals. A worsening CAT score in COPD patients may suggest unreported exacerbations by patients, discontinuation of medications, ineffective intake of treatment, rapid disease progression, or the need for specialist intervention.1,3,4
CAT™ Assessment1,3,4
What is the use of mMRC questionnaire in symptom assessment?
GOLD 2024 states: "the mMRC score relates well to other multidimensional health status measures and predicts future mortality risk". The mMRC questionnaire is used to assess the severity of dyspnea by grading its impact on daily activities on a scale of 0 to 4.1,6 A decrease in mMRC scores indicates successful alleviation of the symptoms.1,6
How does St. George’s Respiratory Questionnaire (SGRQ) help physicians assess COPD patients?
Health Status and QoL are vital outcome parameters that should be assessed in patients with COPD. Perceptions about the impact of symptoms on patient’s QoL may considerably vary between Healthcare Professionals and their patients.10 Tools like the SGRQ, encompassing domains of symptoms, activity, and psychosocial impact, evaluate the effects of COPD on respiratory health and daily life.2,7 With a maximum total score of 100 points, COPD treatment guidelines recommend regular symptomatic treatment in case of SGRQ score ≥25.1,7 A lower score on SGRQ reflects improved health status. A minimum change in SGRQ score of 4 units is considered as clinically relevant.2
What other parameters should be monitored to evaluate treatment success?
According to COPD treatment guidelines, walking tests can be used to evaluate disability and risk of mortality.1 Reduced exercise capacity is associated with disease progression, increasing predisposition to poor QoL, hospitalisation and mortality.1 A six-minute walk test (6MWT) can be performed to assess exercise tolerance.1 An increase in the distance covered during the 6MWT signifies enhanced physical fitness, a key goal to reduce symptoms.12
References
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2024 report). Available at https://goldcopd.org/2024-gold-report/ Accessed 23/07/2024.
- Glaab T, Vogelmeier C, and Buhl R. Outcome measures in chronic obstructive pulmonary disease (COPD): strengths and limitations. Respir Res. 2010;11:79.
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648-54.
- COPD Assessment Test. 2022. Available at https://www.catestonline.org/hcp-homepage/clinical-practice.html Accessed 23/07/2024.
- American Thoracic Society. Surveillance for respiratory hazards in the occupational setting. Am Rev Respir Dis. 1982;126:952-6.
- The modified MRC scale. 2020.Available at https://www.pcrs-uk.org/sites/default/files/resources/MRC-Score.pdf. Accessed 23/07/2024.
- St Georges' University London. St. George's Respiratory Questionnaire for COPD patients (SGRQ-C). 2023. Available at https://www.sgul.ac.uk/research/research-operations/research-administration/st-georges-respiratory-questionnaire/docs/SGRQ-C-English-version.pdf. Accessed 23/07/2024.
- Suissa S, Dell'Anniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67:957-963.
- Halpin DMG, Decramer M, Celli BR, et al. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017;128:85-91.
- Celli B, Blasi F, Gaga M, et al. Perception of symptoms and quality of life - comparison of patients' and physicians' views in the COPD MIRROR study. Int J Chron Obstruct Pulmon Dis.2017;12:2189-2196.
- Leidy NK, et al. Interpreting Evaluating Respiratory Symptoms(TM) in COPD Diary Scores in Clinical Trials: Terminology, Methods, and Recommendations. Chronic Obstr Pulm Dis. 2022;9(4):576-90.
- What to know about the 6-minute walk test. Available at https://www.medicalnewstoday.com/articles/6-minute-walk-test Accessed 24/07/2024.
MAT-XU-2402880 (v1.0) Date of Preparation: January 2025