- Article
- Source: Campus Sanofi
- 25 Jun 2024
Burden of Influenza

What is the burden of influenza for at-risk patients?
Although flu infection may carry risk for any age group, the risk of serious complication due to flu are higher in certain risk groups.1
Adults aged 65 years and over may be at increased risk of flu-related complications as a result of a weakened immune system that occurs with age.1,2 Flu may cause pneumonia and other respiratory complications.2
Patients with certain underlying health conditions may be at increased risk of complications.1,2 Examples of underlying health conditions that may be at increased risk of serious flu-related complications include but are not limited to:
- Chronic respiratory/ heart conditions
- Diabetes
- Immunosuppression
- Neurological conditions
- Obesity
- Kidney disease
- Liver disease
The risk of serious illness from flu is increased during pregnancy as a result of changes to the immune system to support the growing baby.1,2 Vaccination during pregnancy can provide passive immunity to the baby for the first few months of life following birth and can reduce the risk of premature birth and low birth weight.1,2
Adults aged 65 years and over may be at increased risk of flu-related complications as a result of a weakened immune system that occurs with age.1,2 Flu may cause pneumonia and other respiratory complications.2
Patients with certain underlying health conditions may be at increased risk of complications.1,2 Examples of underlying health conditions that may be at increased risk of serious flu-related complications include but are not limited to:
- Chronic respiratory/ heart conditions
- Diabetes
- Immunosuppression
- Neurological conditions
- Obesity
- Kidney disease
- Liver disease
The risk of serious illness from flu is increased during pregnancy as a result of changes to the immune system to support the growing baby.1,2 Vaccination during pregnancy can provide passive immunity to the baby for the first few months of life following birth and can reduce the risk of premature birth and low birth weight.1,2
Flu vaccination is an essential part of helping protect communities2
What are the complications associated with the burden of Influenza?
Flu is an unpredictable virus which can lead to severe complications that can impact people’s lives.3-6*
In the 1–3 days following a laboratory-confirmed influenza infection:a
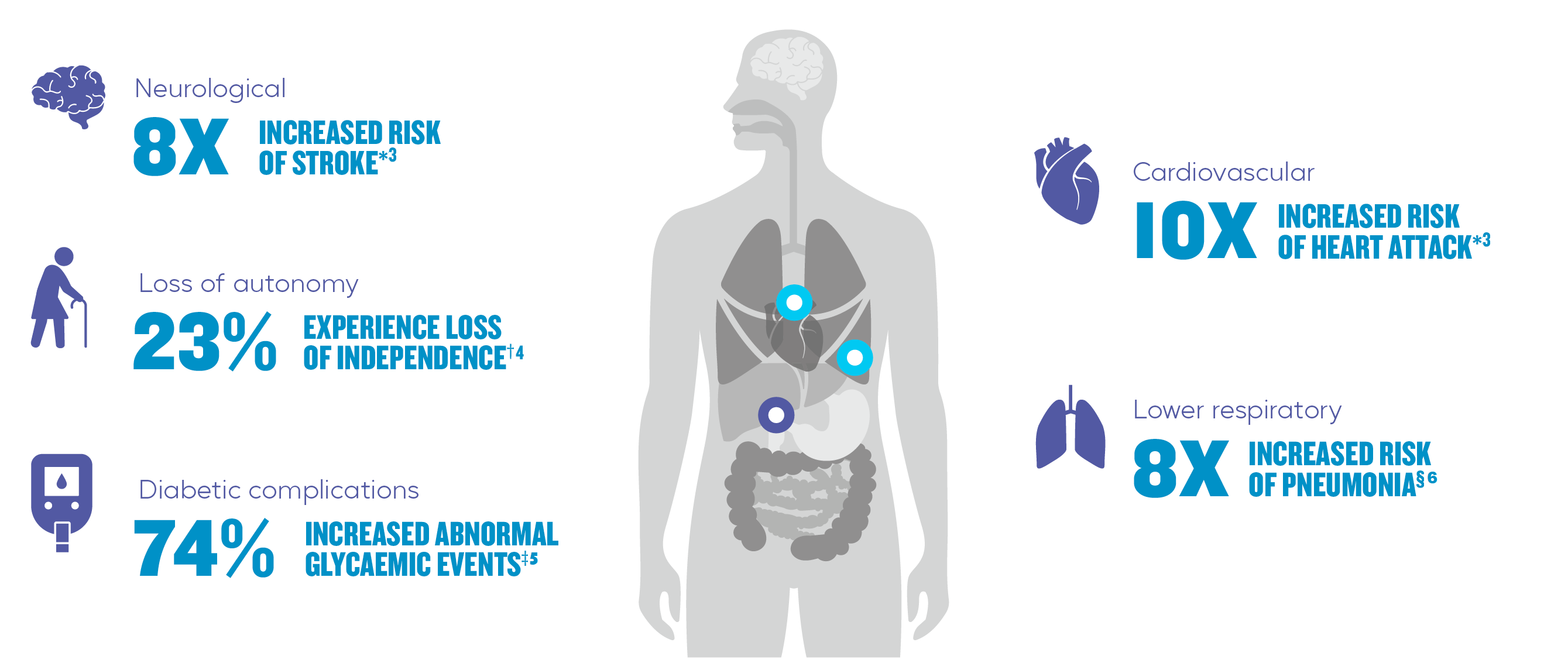
*Scottish case series analysis using national infection surveillance data identifying adults ≥40 years who had a first myocardial infarction (n=1,227) or stroke (n=762) between 1 January 2004 and 31 December 2014.3
†Canadian protective observational cohort study including data from 925 patients aged ≥65 years admitted to hospital with influenza and other acute respiratory infections from 2011 to 2012.4
‡Retrospective cohort analysis of a US health plan comparing 54,656 adults (≥18 years of age) with type 2 diabetes and 113,016 non-diabetic controls.5
§Matched case-control and prospective cohort study among 3,234 Nicaraguan children aged 0-14 years from 2011 to 2018.6
Hospitalisations and economic burden of influenza
Seasonal influenza creates a burden on primary and secondary healthcare services, and the economy7:
- through staff absences, increased demand and wait times, and psychological stress
- through absenteeism, presenteeism and financial loss for patients
- through lost working days
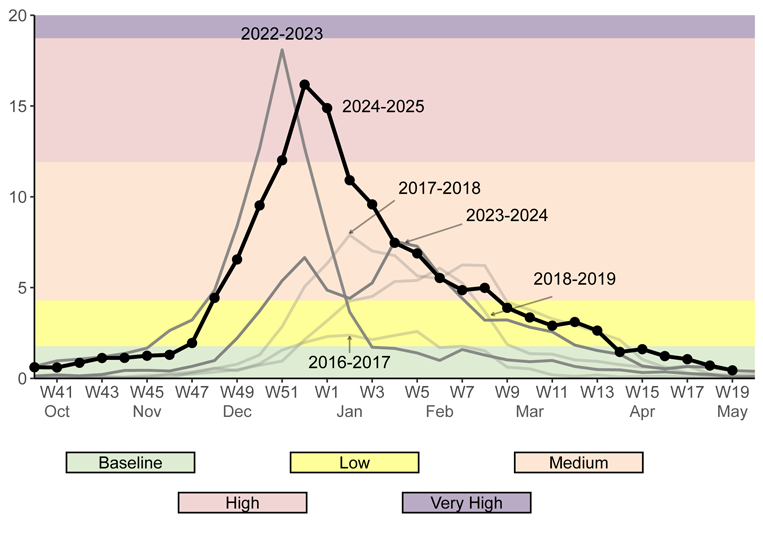
Weekly flu-related hospital admissions for the 2024/2025 season were 14.09 per 100,000 people in England.2 The 2022/2023 flu season recorded 14,500 excess deaths associated with flu in England.8,9 See below a graph of hospital admission rates per 100,000 population:
Influenza may have a considerable burden on secondary healthcare systems.10

Hospital admissions during the 2022/23 season influenza season had associated medical costs of ~140M*.10,11
*Average cost per hospital admissions comes from Moss et al.8 The total influenza hospital admission rate per 100,000 over the period week 35, 2022 to week 9, 2023 comes from the National influenza and COVID-19 surveillance reports for the 2022-2023 season.11
Certain groups may create increased pressure as they are more likely to experience a longer and more severe illness. Data below is derived from an average of 2017/18 and 2018/19 season costs from Moss et al:
| <65 years |
75+ years |
|
Costs per hospitalisation: ~£1,900 |
Costs per hospitalisation: ~£3,700 |
|
Average length of stay: 4.74 days |
Average length of stay: 12.55 days |
|
Mortality: 1.83% |
Mortality: 11.18% |
This highlights the importance of vaccination to reduce flu-related complications and associated burden on healthcare systems:
Influenza vaccines can help protect your appropriate patients, including some of the most at-risk, from flu-related complications.
Learn more about Sanofi Influenza Vaccines :

Supemtek TIVr ▼ (Trivalent Influenza Vaccine (recombinant, prepared in cell culture))
Learn more about Supemtek TIVr and the potential to help simplify your flu campaign.
References
- Influenza: the green book, chapter 19. Available at: Influenza: the green book, chapter 19 - GOV.UK Accessed June 2025
- UKHSA. Flu vaccine. The flu vaccination: who should have it and why (winter 2024 to 2025) - GOV.UK Accessed June 2025
- Warren-Gash C, et al. Eur Respir J 2018;51:1701794
- Andrew M K, et al. J Am Geriatr Soc 2021;69:696-703
- Samson S I, et al. J Diabetes Sci Technol 2021;15:44-52
- Kubale J, et al. Clin Infect Dis 2021;73:e4288-e4295
- Romanelli RJ et al. The societal and indirect economic burden of seasonal influenza in the United Kingdom. RAND Corporation. Available atr: rand.org Accessed June 2025
- GOV.UK. National flu and COVID-19 surveillance report. Last updated 28 March 2025. Available at: gov.uk. Accessed June 2025
- UK Health Security Agency. Press release. Excess deaths associated with flu highest in 5 years, 22 June 2023. Available at: gov.uk. Accessed June 2025
- Moss JWE, et al. BMC publish Health. 2020;20(1):1464
- UKHSA. SUrveillance of influenza and other seasonal respiratory viruses in the UK, winter 2022 to 2023. Available at: https://www.gov.uk/government/statistics/annual-flu-reports/surveillance-of-influenza-and-other-seasonal-respiratory-viruses-in-the-uk-winter-2022-to-2023 Accessed June 2025
MAT-XU-2301387 (v4.0) Date of preparation: June 2025