- Article
- Source: Campus Sanofi
- 16 Sept 2025
The Importance of Glycaemic Control: Strategies to Support People with Type 2 Diabetes

This article series is intended for diabetes specialist nurses and primary care physicians.
Table of Contents
- The Challenges in Glycaemic Control Conversations
- Why Glycaemic Control Matters: Beyond the Numbers
- Practical Strategies for Effective Engagement
- Holistic Approaches to Glycaemic Control
- Key Long-Term Benefits of Type 2 Diabetes Management
- Tailoring Your Approach
- Conclusion: Empowering Patients Through Clear Communication
- Explore More
The Challenges in Glycaemic Control Conversations
Glycaemic control plays a fundamental role in Type 2 Diabetes management. However, patients may encounter barriers that may impede optimal glucose management, including1,2:

Through the implementation of communication strategies, clinical encounters can be transformed into constructive therapeutic dialogues that enhance patient engagement and promote active participation in Type 2 Diabetes self-management.1,2
Why Glycaemic Control Matters: Beyond the Numbers
When discussing glycaemic control with patients, translating clinical terms like HbA1c into real-life benefits can greatly enhance their motivation and engagement.
Patients who maintain optimal glycaemic control report3:
- Improved quality of life
- Fewer diabetes related symptoms, such as polydipsia and polyuria
While HbA1c levels remain a cornerstone measurement of long-term glycaemic control, introducing patients to Time-in-Range (TIR) can offer a more comprehensive view of their overall glycaemic status.4,5
- TIR is now recognised by major diabetes organisations including the American Diabetes Association (ADA), and the European Association for the Study of Diabetes (EASD) as a valuable complementary metric.5
- Patients may find it encouraging to learn that even modest improvements in TIR (as little as 5%) are associated with clinically meaningful benefits.5
- Research shows many patients perceive starting insulin therapy as a personal setback believing it means they haven't managed their Type 2 Diabetes well. This misconception can create a significant psychological barrier to accepting treatment.1,6
- By reframing insulin as a natural and necessary step in the progression of Type 2 Diabetes management, you can help patients feel more empowered and open to starting insulin therapy.
Reluctance to escalate treatment despite evident clinical indicators constitutes a significant obstacle in optimal Type 2 Diabetes management.7 This postponement frequently stems from a mixture of both clinician reservation and patient apprehension.7
Through recognition of this phenomenon and implementation of effective communication strategies, clinicians can facilitate patients' attainment of glycaemic targets more expeditiously, potentially enhancing long-term clinical outcomes.7
Practical Strategies for Effective Engagement
Employing empathetic, objective communication can facilitate positive patient perceptions of insulin therapy and other therapeutic interventions.8
To make complex concepts more understandable, consider using:
- Visual representation tools
- Analogies and comparative frameworks
- Contextually relevant and relatable examples
- Allocate consultation time to explore individual concerns, preconceptions, and apprehensions regarding therapeutic options.
- Implementing targeted inquiry such as like, "What aspects of insulin initiation concern you the most?" can facilitate meaningful conversations that might otherwise never happen.10
Holistic Approaches to Glycaemic Control
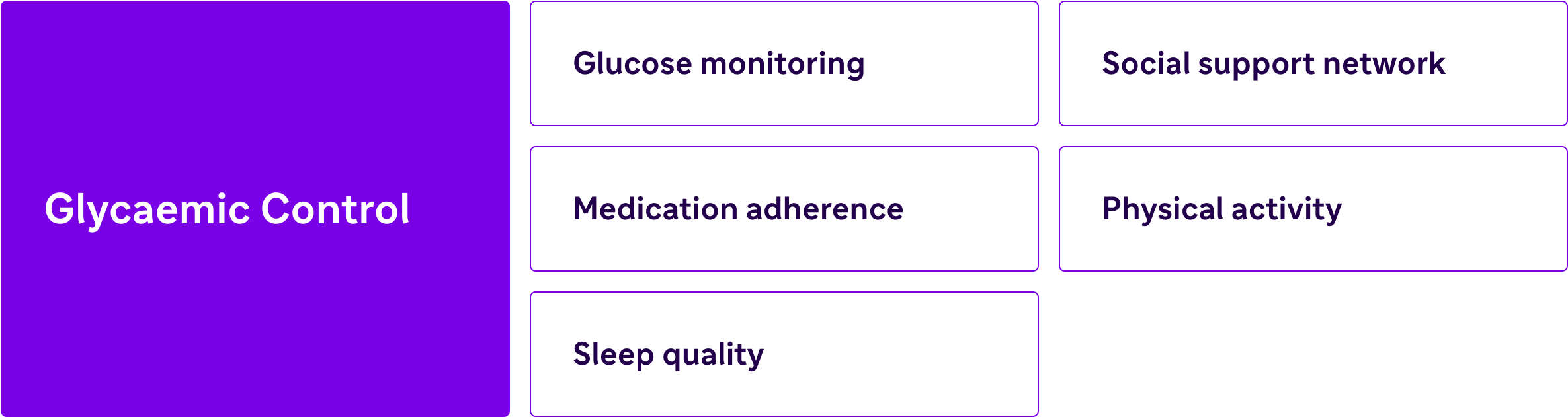
- While medication adherence is essential for maintaining glycaemic control,11 lifestyle interventions constitute a component of comprehensive diabetes management.12
- Educate patients that consistent physical activity enhances insulin sensitivity, emphasising that even moderate adjustments can yield significant clinical improvements.13
- Consider the impact of sleep quality: clinical evidence demonstrates that inadequate sleep patterns adversely affect blood glucose regulation.14
Integrating these lifestyle factors with pharmacological approaches can facilitate more efficacious and sustainable therapeutic outcomes.14
Social support networks are instrumental in facilitating effective diabetes self-management.15 Including family members with consent in educational interventions, when appropriate, enhances comprehension and promotes collective responsibility. Furthermore, facilitating connections with diabetes support communities provides both psychological reinforcement and practical strategies.15 These relationships frequently contribute to improved therapeutic adherence and enhanced self-efficacy in condition management.15
Blood glucose self-monitoring serves as a critical component in optimising glycaemic control by providing immediate feedback and establishing clear associations between daily activities and clinical outcomes.16 For appropriate candidates, highlighting the advantages of continuous glucose monitoring systems can enhance this approach by delivering comprehensive, real-time data and clinically relevant insights.17
Key Long-Term Benefits of Type 2 Diabetes Management
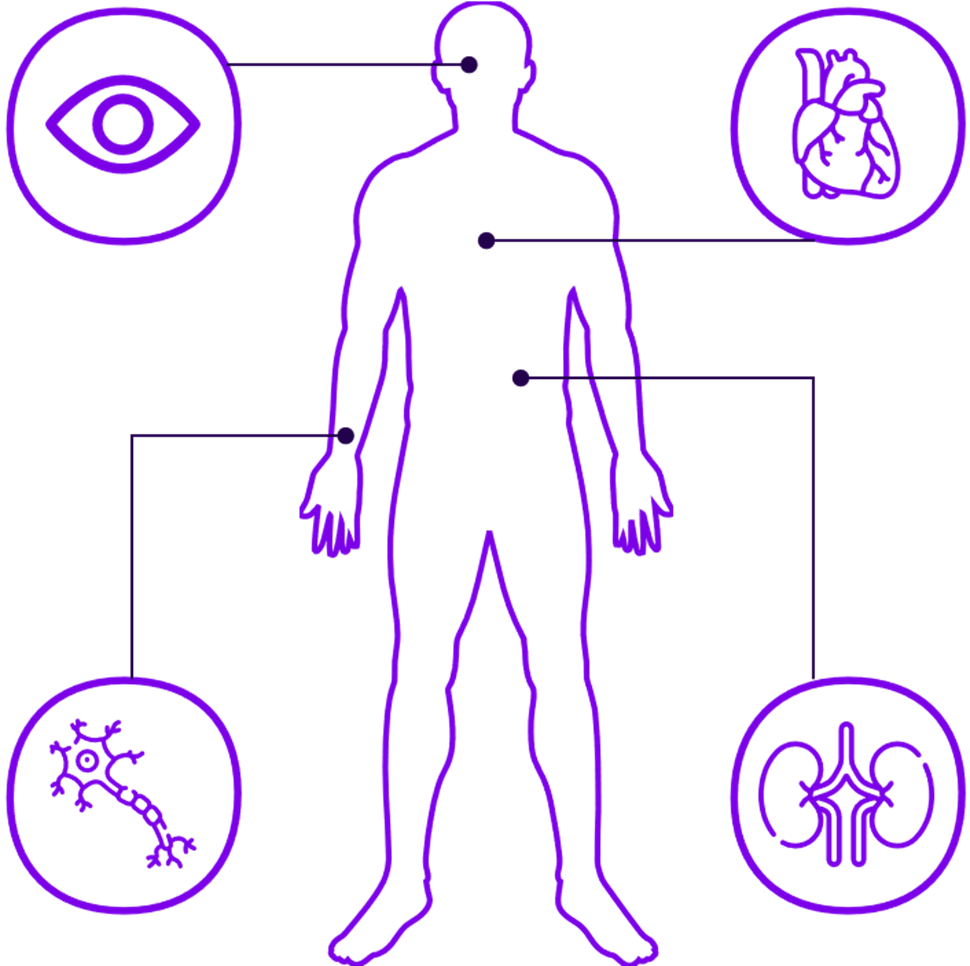
- Optimal glycaemic control demonstrates significant efficacy in reducing microvascular complications of diabetes, preserving the integrity and function of critical organ systems.18
- This clinical benefit translates into tangible patient outcomes when individuals understand that consistent glycaemic management directly preserves retinal, renal, and neurological function, transforming abstract control targets into meaningful health preservation strategies.18
Research demonstrates that early implementation of intensive glucose control yields sustained cardiovascular benefits.19 This phenomenon, known as "metabolic memory," emphasises the clinical imperative of establishing optimal glycaemic control in the early disease course to mitigate cardiovascular risk.19
Tailoring Your Approach
Evidence supports the individualisation of HbA1c targets based on specific clinical parameters20:
- Age
- Comorbidities
- Diabetes duration and hypoglycaemic risk
Engaging in evidence-based discussions regarding target individualisation facilitates patient comprehension of their tailored therapeutic approach, potentially enhancing treatment adherence and clinical outcomes.
- Diabetes significantly impacts psychosocial well-being, with affected individuals experiencing elevated levels of disease-related distress. Clinical evidence indicates an approximate 2-fold increase in depression and anxiety disorders among individuals with Type 2 Diabetes compared to population norms.21
- Consequently, vigilant glycaemic monitoring becomes particularly crucial in patients exhibiting depressive symptoms. Comprehensive management protocols should integrate psychological support mechanisms and enhanced self-management strategies.21
Conclusion: Empowering Patients Through Clear Communication
When insulin is appropriate, it becomes fundamental for ensuring optimal long-term health outcomes. This clinical journey begins with effective communication strategies. Facilitate patient comprehension regarding glycaemic control through evidence-based explanations, addressing psychological resistance factors, and implementing individualised support protocols. These methodical approaches can enhance therapeutic dialogues about glycaemic management importance in Type 2 Diabetes patients.
Each clinical encounter presents an opportunity to establish rapport and enhance patient literacy. The clinical support above can significantly influence patients' long-term health trajectories.
Explore More
- Polonsky WH, Capehorn M, Belton A, et al. Physician-patient communication at diagnosis of Type 2 Diabetes and its links to patient outcomes: new results from the global IntroDia® study. Diabetes Res Clin Pract. 2017;127:265-274. doi:10.1016/j.diabres.2017.03.016
- Khunti K, Zaccardi F, Amod A, et al. Glycaemic control is still central in the hierarchy of priorities in Type 2 Diabetes management. Diabetologia. 2025;68(1):17-28. doi:10.1007/s00125-024-06254-w
- Testa MA, Simonson DC. Health economic benefits and quality of life during improved glycaemic control in patients with type 2 diabetes mellitus: a randomised, controlled, double-blind trial. JAMA. 1998;280(17):1490-1496. doi:10.1001/jama.280.17.1490
- Sun B, Luo Z, Zhou J. Comprehensive elaboration of glycaemic variability in diabetic macrovascular and microvascular complications. Cardiovasc Diabetol. 2021;20(1):9. doi:10.1186/s12933-020-01200-7
- Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the International consensus on time in range. Diabetes Care. 2019;42(8):1593-1603. doi:10.2337/dci19-0028
- Brod M, Alolga SL, Meneghini L. Barriers to initiating insulin in Type 2 Diabetes patients: development of a new patient education tool to address myths, misconceptions and clinical realities. Patient. 2014;7(4):437-450. doi:10.1007/s40271-014-0068-x
- Reach G, Pechtner V, Gentilella R, et al. Clinical inertia and its impact on treatment intensification in people with Type 2 Diabetes mellitus. Diabetes Metab. 2017;43(6):501-511. doi:10.1016/j.diabet.2017.06.003
- Dickinson JK, Guzman SJ, Maryniuk MD, et al. The use of language in diabetes care and education. Diabetes Care. 2017;40(12):1790-1799. doi:10.2337/dci17-0041
- Essien O, Otu A, Umoh V, et al. Intensive patient education improves glycaemic control in diabetes compared to conventional education: a randomised controlled trial in a Nigerian tertiary care hospital. PLoS One. 2017;12(1):e0168835. doi:10.1371/journal.pone.0168835
- Holmes-Truscott E, Browne JL, Ventura AD, et al. Diabetes stigma is associated with negative treatment appraisals among adults with insulin-treated Type 2 diabetes: results from the second Diabetes MILES - Australia (MILES-2) survey. Diabet Med. 2018;35(5):658-662. doi:10.1111/dme.13598
- Khunti K, Wolden ML, Thorsted BL, et al. Clinical inertia in people with type 2 diabetes: a retrospective cohort study of more than 80,000 people. Diabetes Care. 2013;36(11):3411-3417. doi:10.2337/dc13-0331
- American Diabetes Association. Lifestyle Management. Diabetes Care. 2017;40(Suppl 1):S33-S43. doi:10.2337/dc17-S007
- Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065-2079. doi:10.2337/dc16-1728
- Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018;84:56-66. doi:10.1016/j.metabol.2018.02.010
- Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep. 2012;12(6):769-781. doi:10.1007/s11892-012-0317-0
- Polonsky WH, Fisher L, Schikman CH, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the structured testing program study. Diabetes Care. 2011;34(2):262-267. doi:10.2337/dc10-1732
- Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous Glucose Monitoring Versus Usual Care in Patients With Type 2 Diabetes Receiving Multiple Daily Insulin Injections: A Randomized Trial. Ann Intern Med. 2017;167(6):365-374. doi:10.7326/M16-2855
- Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with Type 2 Diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837-853.
- Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577-1589. doi:10.1056/NEJMoa0806470
- American Diabetes Association Professional Practice Committee; Glycaemic goals and hypoglycaemia: standards of care in diabetes—2024. Diabetes Care 47 (Supplement_1): S111–S125. https://doi.org/10.2337/dc24-S006
- Roy T, and Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142 Suppl:S8-S21. doi:10.1016/S0165-0327(12)70004-6
MAT-XU-2503071-1.0-09/2025
