- Article
- Source: Campus Sanofi
- May 1, 2025
The Spectrum of Gaucher Disease Symptoms
Signs and Symptoms
Understanding the spectrum
Gaucher disease signs and symptoms are diverse, unpredictable, and variable.1
Gaucher presents on a spectrum of symptoms. This means there is a range of symptoms and symptom severity that people may experience. Some may have long periods of time when little or no symptoms are present. Others may experience only bone (skeletal) or organ-related symptoms. Certain individuals may have central nervous system-related (neuronopathic) symptoms. Gaucher is a lifelong condition no matter what symptoms a patient may present with.1
The symptoms and how Gaucher develops may not be the same for everyone, even for people in the same family.2 |
Spectrum of Gaucher disease symptoms
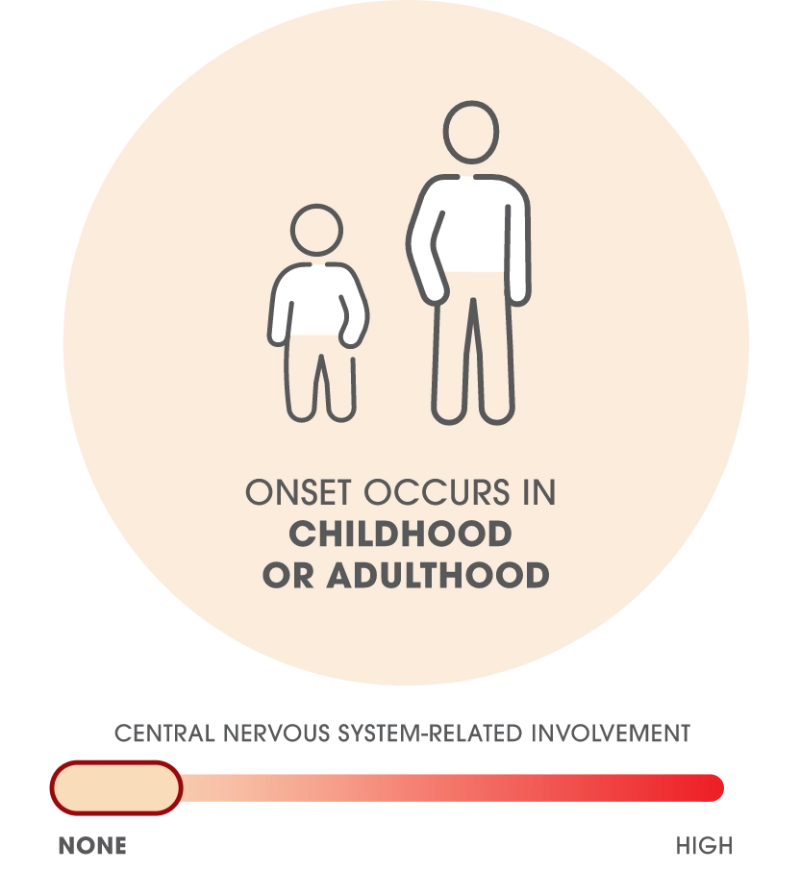
TYPE 1
NON-NEURONOPATHIC FORM
.png)
Patients may experience no symptoms, a combination of symptoms, or all symptoms.2 56% of patients may experience symptoms before 20 years of age.3
Visceral (Organs)3,4
- Splenomegaly and/or Hepatomegaly with abdominal pain or distension
- Liver Fibrosis can develop as disease progresses
Hematologic (Blood)2,5
- Anemia (leading to fatigue)
- Thrombocytopenia leading to easy bruising or bleeding
Skeletal (Bone)7
- In most patients with Gaucher disease, various manifestations of bone disease progress over years, presenting as chronic or acute bone pain, bone crisis, bone marrow infiltration, bone mineral reduction, osteonecrosis, pathologic fracture, growth delay, and/or Erlenmeyer flask deformity. 82% of patients with Gaucher disease have radiographic evidence of bone disease.
Some patients with Gaucher disease type 1 may not notice symptoms. These patients may still have effects of the disease such as cytopenia, hepatosplenomegaly, or certain bone manifestations.8 |
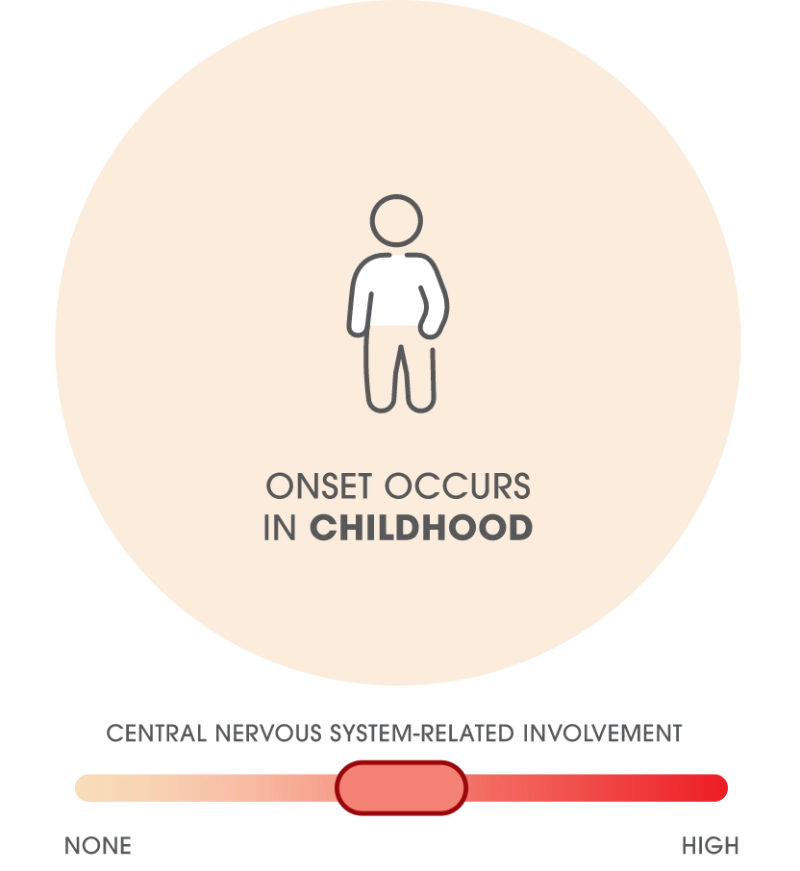
TYPE 3
CHRONIC NEURONOPATHIC FORM
.png)
Patients with Gaucher disease type 3 typically exhibit early onset of severe hematological and visceral disease and growth delay throughout childhood, which can be accompanied or followed by the development of neurological symptoms. Approximately 50% of patients will display some signs of neurological manifestations by 2 years of age.9,10
While gaze palsy is the hallmark of Gaucher disease type 3, its absence does not rule out a diagnosis.11-14
Central nervous system, variable onset
- Eye abnormalities, which are observed as gaze palsy with markedly slow or absent horizontal saccades14
- Movement disorders, which are observed as ataxia, seizures, myoclonic epilepsy, tremor, and/or dystonia14
Other features suggestive of gaucher disease type 3
- Kyphosis15
- Lung disease15
- Lymphadenopathy15
- Gaucheromas15
- Cognitive symptoms, manifesting as a spectrum ranging from mild cognitive impairment to severe intellectual disability16
- Hyperreflexia, where exaggerated deep tendon reflexes are observed17
- Bulbar disorders, which are observed as stridor, dysphagia, and/or dysarthria15
The distinction between Gaucher disease type 1 and type 3 is not straightforward, and patients should be frequently assessed for emergence of neurological symptoms during the course of their disease.18-21 |
TYPE 2
ACUTE INFANTILE NEURONOPATHIC FORM
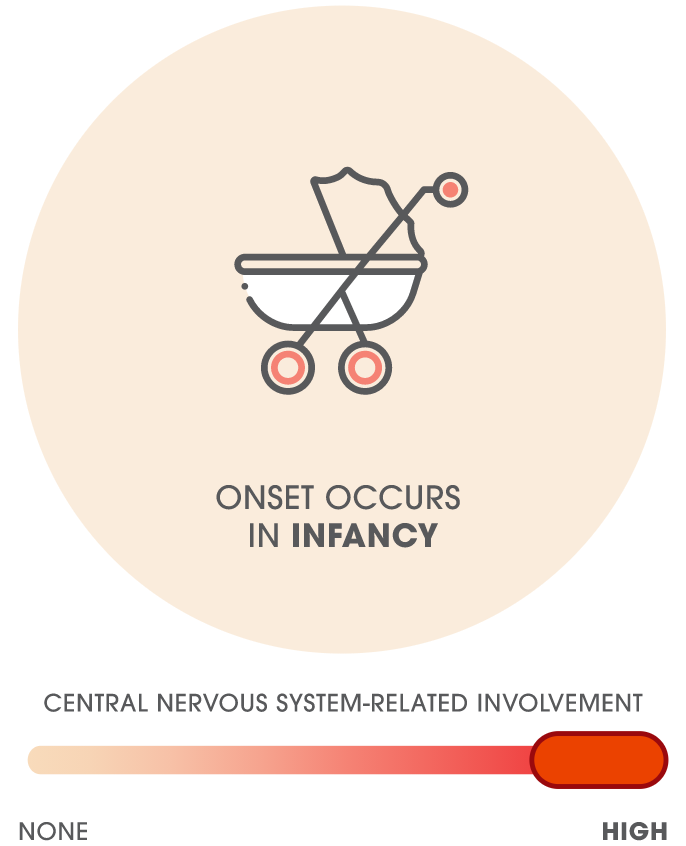
Patients with Gaucher disease type 2 have early onset of central nervous system symptoms by 6 months of age and rapid nervous system decline in the first 2 years of life.15 These patients can also exhibit the visceral and hematologic symptoms seen in type 1 patients.5
Central nervous system, early onset
- Severe stridor and apnea15
- Failure to achieve independent gait14
- Developmental delay and worsening cognitive decline5
- Poor weight gain5
- Feeding difficulties due to abnormal swallowing, often requiring tube feedings5
- Development of spasticity, opisthotonus and/or progressive myoclonic epilepsy5
- Supranuclear gaze palsy or convergent squint12
- Visceral and hematologic symptoms seen in type 1
References: 1. Sidransky E. Gaucher Disease: Practice Essentials, Background, Pathophysiology. Medscape. Updated October 5, 2023. Accessed July 22, 2025. https://emedicine.medscape.com/article/944157-overview 2. Pastores GM et al. Semin Hematol. 2004;41(4 Suppl 5):4-14. 3. Stirnemann J et al. Int J Mol Sci. 2017;18(2):441. 4. Charrow J et al. Arch Intern Med. 2000;160(18):2835-2843. 5. Grabowski GA et al. The Online Metabolic and Molecular Bases of Inherited Disease. Accessed March 11, 2024. https://ommbid.mhmedical.com/content.aspx?bookid=2709§ionid=225546056 6. Mikosch PK et al. Wien Med Wochenschr. 2010;160(23-24):609-624. 7. Goker-Alpan O. Mol Genet Metab. 2011;104(4):438-447. 8. Mistry PK et al. Am J Hematol. 2011;86(1):110-115. 9. El-Beshlawy A et al. Mol Genet Metab. 2017;120(1-2):47-56. 10. Tylki-Szymańska A et al. J Inherit Metab Dis. 2010;33(4):339-346. 11. Gary SE et al. Expert Rev Endocrinol Metab. 2018;13(2):107-118. 12. Mistry PK et al. Mol Genet Metab. 2017;120(1-2):8-21. 13. Lu WL et al. Orphanet J Rare Dis. 2023;18(1):293. 14. Zhong W et al. Acta Neurol Belg. 2024;124(4):1213-1223. 15. Schiffmann R et al. J Inherit Metab Dis. 2020;43(5):1056-1059. 16. Daykin EC et al. Mol Genet Metab. 2021;132(2):49-58. 17. Cleveland Clinic. Hyperreflexia: What It Is, Causes, Symptoms & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/24967-hyperreflexia. Accessed July 23, 2025. 18. Capablo JL et al. J Neurol Neurosurg Psychiatry. 2008;79:219-222. 19. Giraldo P et al. Orphanet J Rare Dis. 2012;7(17):1-10. 20. Giraldo P et al. Blood Cells Mol Dis. 2016;56(1):23-30. 21. Tajima A et al. Mol Genet Metab.2009;97:272-277.
MAT-US-2509009-v1.0-08/2025