- Article
- Source: Campus Sanofi
- 8 May 2025
Inside Atopic Dermatitis: Burden on Patients
_430x268.jpg)
Current treatment options and unmet needs of Atopic Dermatitis
AD is a chronic heterogeneous inflammatory condition characterized by recurrent eczematous lesions and impaired skin barrier function, with multiple immune pathways involved in the pathologic outcomes1-6:
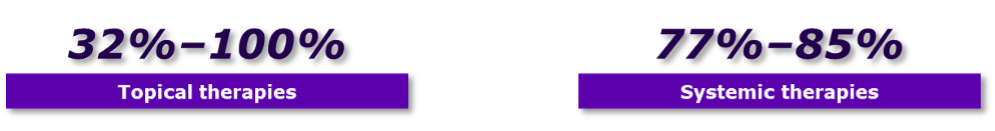
A systematic review suggested that adherence to treatments in patients with AD varied widely for topical and systemic therapies7
Treatment adherence is multidimensional
• Patient-related factors are demographic, socioeconomic, and psychological (e.g. mental health, forgetting)
• Treatment-related factors include route of administration (e.g. adherence is better for oral than for topical therapy) and other factors involving treatment burden (i.e. duration, dosing frequency, regimen complexity, and pill burden), as well as side effects and cost
• Disease-related factors include the chronicity of a skin disease; patients with acute illness are more likely to adhere to treatment than patients with chronic illness
• Physician-related factors include whether patients feel included in the decision-making process of their treatment as opposed to a paternalistic relationship between physician and patient, which does not usually promote adherence
Current treatment options
1. Topical corticosteroid therapy is the mainstay of anti-inflammatory treatment in adults and children with AD8,9
• It is estimated that approximately 10% of adult patients with AD do not respond adequately to topical therapies8,a
• Recommended for adults with ADa: Topical corticosteroids are commonly used as first-line treatment for mild-to-severe dermatitis in all skin regions
• Recommend intermittent use of medium-potency topical corticosteroids as maintenance therapy (2 times per week) to reduce disease flares and relapse
Barriers for topical therapies:
• Topical therapies carry a treatment burden of multiple administrations in a day, although the frequency of application for topical corticosteroids may be limited by the potential for systemic absorption9,11-13
• Topical therapies may be difficult to use in patients with high BSA involvement14
• Application site tolerability issues include burning, pain, stinging, and pruritus15,16
• TCS-specific AEs include purpura, telangiectasia, striae, focal hypertrichosis, acneiform or rosacea-like eruptions, and skin atrophy8,9
2. Systemic therapies are considered for adult patients whose AD is refractory to optimized topical therapy17
• Initiating systemic therapies should be a shared decision between patients and clinicians, considering severity of AD, its impact on the patient, and efficacy, safety, and accessibility of the available therapies
• Strongly recommend the use of biologics and JAK inhibitors
• Conditionally recommend the use of immunosuppressants with proper monitoring of adverse events
o Recommend against the use of systemic corticosteroids
o Use of systemic corticosteroids should be reserved exclusively for acute, severe exacerbations and as a short-term bridge therapy to other systemic corticosteroid-sparing therapy
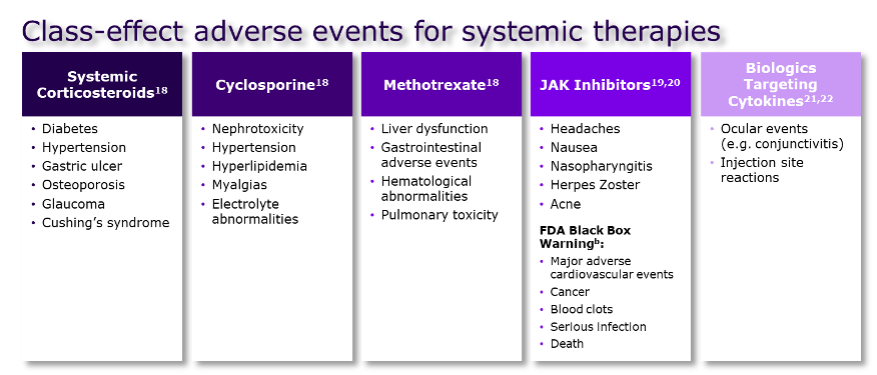
• Limitations of existing systemic therapies
aThis data is from prior to the availability of biologics and therefore may underestimate the true rate of inadequate response.
bEU use restricted based on recommendations from the Pharmacovigilance Risk Assessment Committee.
JAK, Janus kinase
- Langan S, et al. Lancet. 2020;396(10247):345-360;
- Brunner PM, et al. J Allergy Clin Immunol. 2017;139(4S):S65-S76;
- Yang G, et al. Int J Mol Sci. 2020;21(8):2867;
- Girolomoni G, et al. Ther Adv Chronic Dis. 2021;12:20406223211002979;
- Salava A, et al. Clin Transl Allergy. 2014;4:33;
- Schonmann Y, et al. J Allergy Clin Immunol Pract. 2020;8(1):248-257.e16.
- Eicher L, et al. J Eur Acad Dermatol Venereol. 2019;33(12):2253-2263.
- Sidbury R, et al. J Am Acad Dermatol. 2023;89(1):e1-e20;
- Eichenfield LF, et al. J Am Acad Dermatol. 2014;71(1):116-132.
- Lynde CW, et al. J Cutan Med Surg. 2018;22(1):78-83;
- Boguniewicz M, et al. Ann Allergy Asthma Immunol. 2018;120(1):10-22.e2;
- Buys LM. Am Fam Physician. 2007;75(4):523-528;
- Pariser D. Am J Ther. 2009;16(3):264-273;
- Augustin M, et al. Acta Derm Venereol. 2022;102:adv00830;
- Draelos ZD, et al. Dermatol Ther (Heidelb). 2019;9(1):71-102;
- Kim BS, et al. J Allergy Clin Immunol. 2020;145(2):572-582;
- Davis DMR, et al. J Am Acad Dermatol. 2024;90(2):e43-e56.
- Megna M, et al. Dermatol Ther (Heidelb). 2017;7(1):1-23;
- Chang PH, et al. J Dermatol. 2021;48(11):1631-1639;
- Samuel C, et al. Dermatol Ther (Heidelb). 2023;13(3):729-749;
- Martora F, et al. J Dermatolog Treat. 2024;35(1):2304027;
- Alraddadi R, et al. JAAD Int. 2023;13:46-47.
- ICER. JAK Inhibitors and Monoclonal Antibodies for the Treatment of Atopic Dermatitis: Final Policy Recommendations. August 17, 2021. Accessed March 29, 2024. https://icer.org/wp-content/uploads/2020/12/Atopic-Dermatitis_Policy-Recommendations.pdf;
- Drucker AM, et al. Dermatitis. 2022;33(3):200-206;
- Tang T, et al. J Allergy Clin Immunol. 2014;133(6):1615-1625.e1;
- Abuabara K, et al. Dermatol Clin. 2017;35(3):291-297;
- Le M, et al. Front Med (Lausanne). 2021;8:682547;
- Eichenfield LF, et al. Dermatol Ther (Heidelb). 2020;10(4):791-806
MAT-BH-2600012