- Article
- Source: Campus Sanofi
- 8 May 2025
Mechanism of Action of Atopic Dermatitis
_430x268.jpg)
Atopic Dermatitis Mechanism of Disease Webpage
Atopic Dermatitis Pathophysiology1,2:
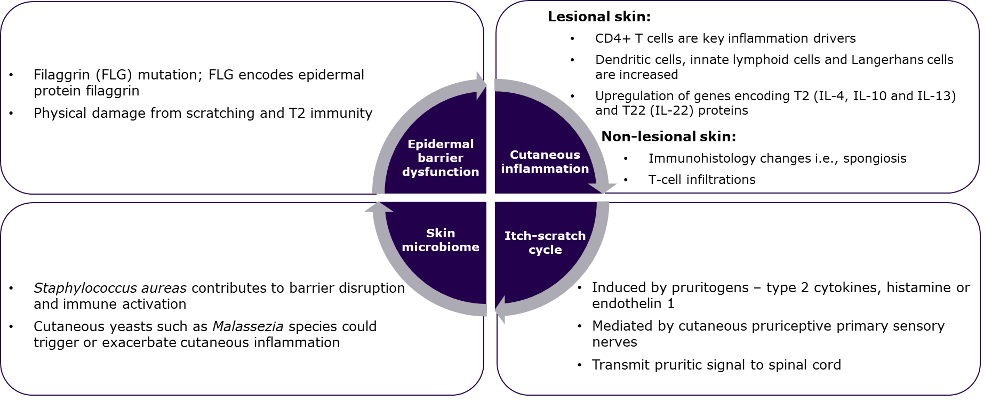
Figure 1: Life Cycle of Atopic Dermatitis1,2
Epidermal Barrier dysfunction1-3:
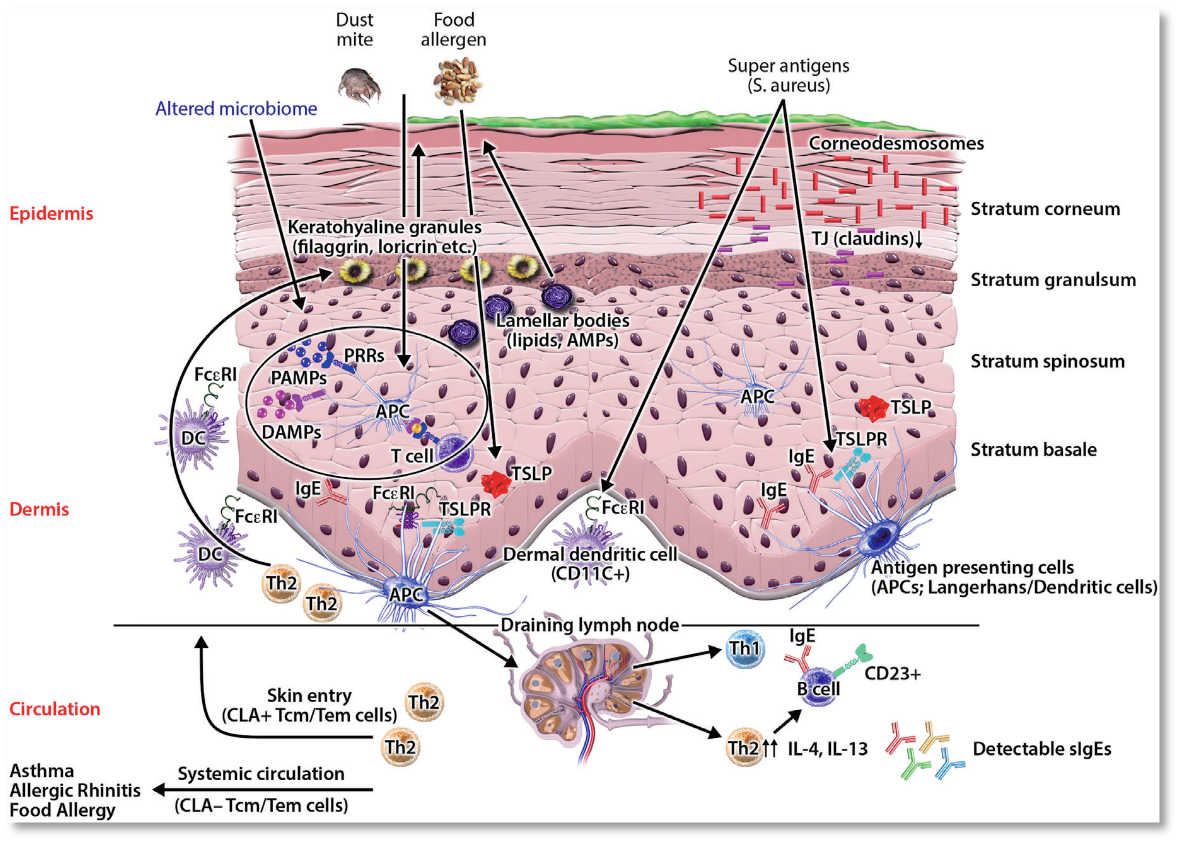
Figure 2: Pathophysiology- Epidermal barrier dysfunction,1-3
|
Mechanism2 • Primary: FLG mutations; secondary: Itch-scratch cycle • Reduced expression of epidermal structural proteins or lipids in response to T2 and T22 cytokines1,2
|
Epidermal changes1-3 • Increased pH • Trans epidermal water loss • Easy irritability • Increased permeability • Increased susceptibility to infection • Altered lipid composition |
|
EBD promotes inflammation2 • Dysregulation of immunomodulatory proteins • Release of DAMPs • Release of alarmins and cytokines -IL-1β, IL-4, IL-13, IL-25, IL-17A, IL-33 and TSLP
|
Molecular changes1-3 • Abundance of Staphylococcus aureas and Malassezia yeasts • T2 mediated downregulation of skin barrier genes and stratum corneum lipids • Keratinocytes send pro-inflammatory and pruritogenic signals • Reduced expression of tight junction proteins |
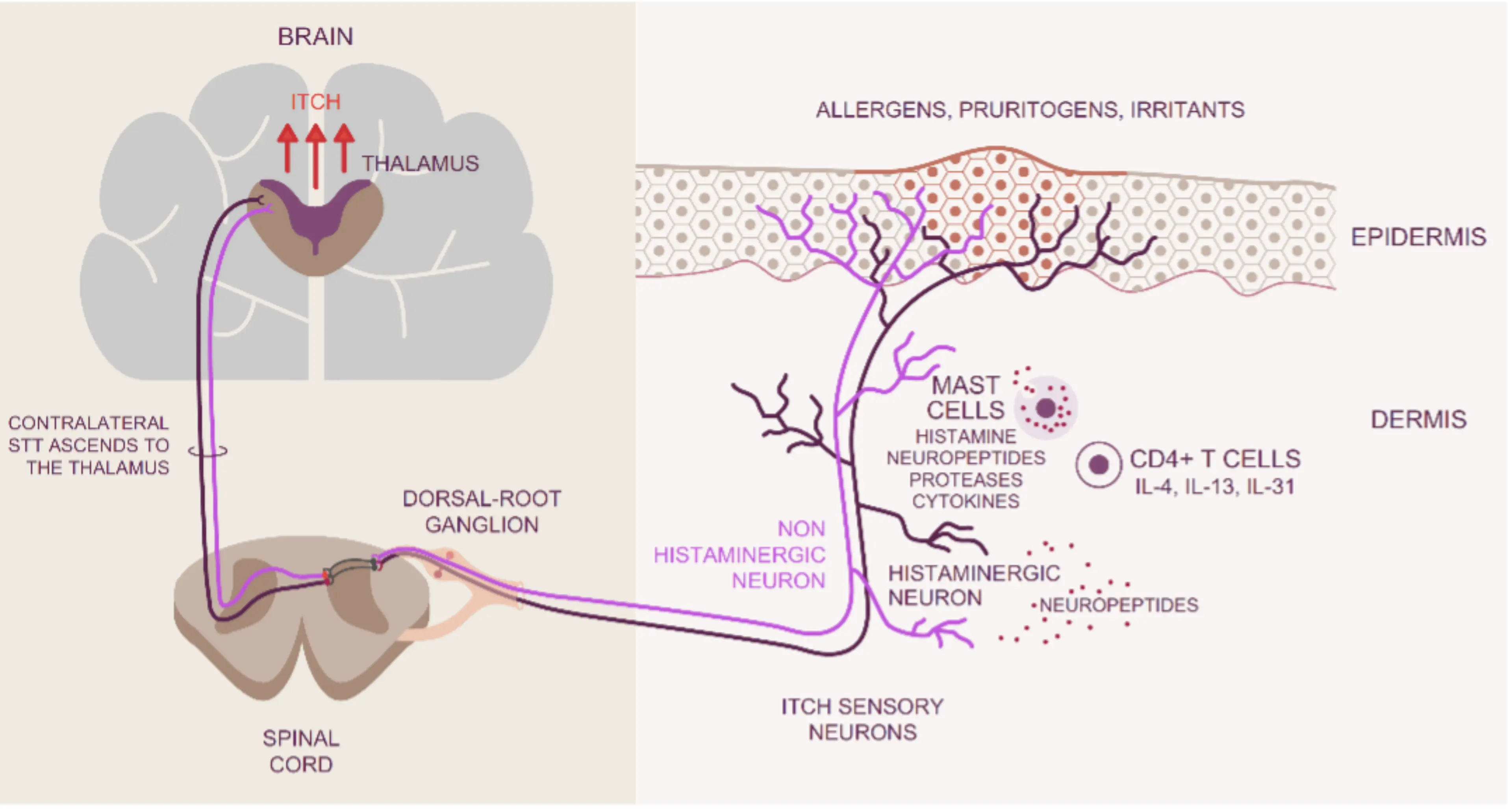
Itch-scratch Cycle1,2,4:
|
|
Figure 3: Pathophysiology- Itch-scratch cycle1,2,4
• Induced by pruritogens - antigens, histamines, endothelin 1, T2 cytokines1,2,4
• Sensory nerves transmit signals to spinal cord1,2,4
• Pathways: Histamine-dependent or independent and T2 signaling1,2,4
• T2 cytokines (IL-4, IL-13, TSLP and IL-31) contribute to itch1
• TSLP released by keratinocytes activate TRPA1 and T2 cytokines stimulate afferent neurons through IL-4 alpha and JAK1 2
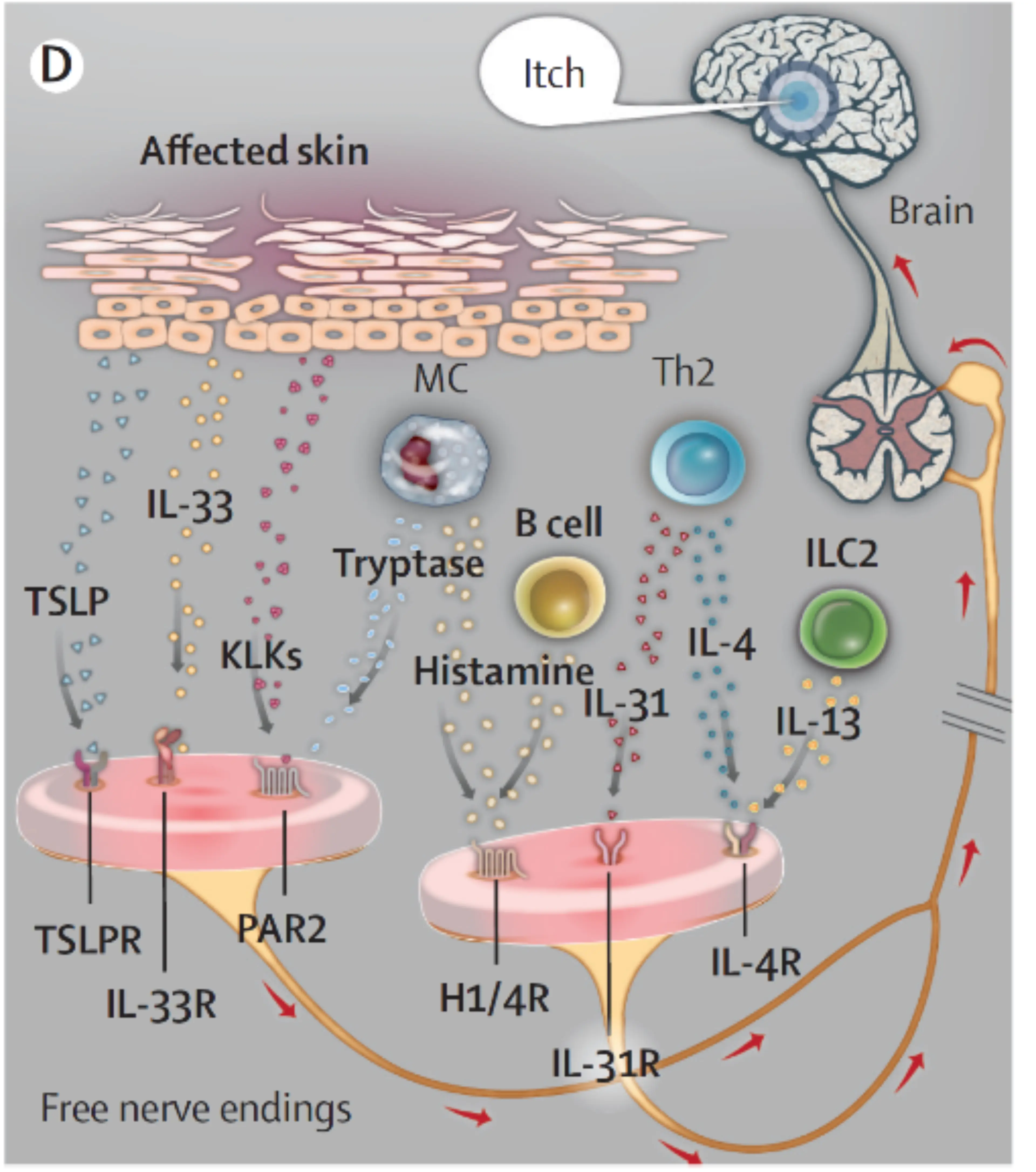
Microbiome1,2
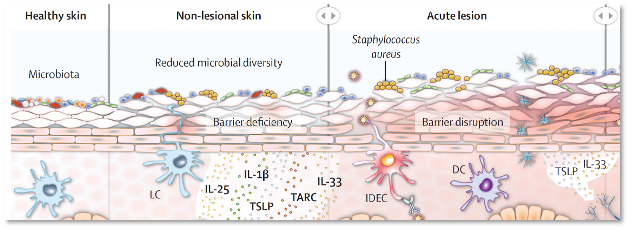
Figure 4: Microbiome1,2
• One of the functions of the normal skin microbiota is suppression of Staphylococcus aureus growth1.2
• Decreased microbiota favor Staphylococcus and S. aureus in particular2
• Staphylococcus aureus commonly found on skin of patients with AD; 30-100% depending on age and disease severity1,2
• Staphylococcus aureus expresses numerous virulence factors through keratinocytes and immune cells1,2,5
• In addition, yeasts, Malassezia can directly stimulate skin inflammation2
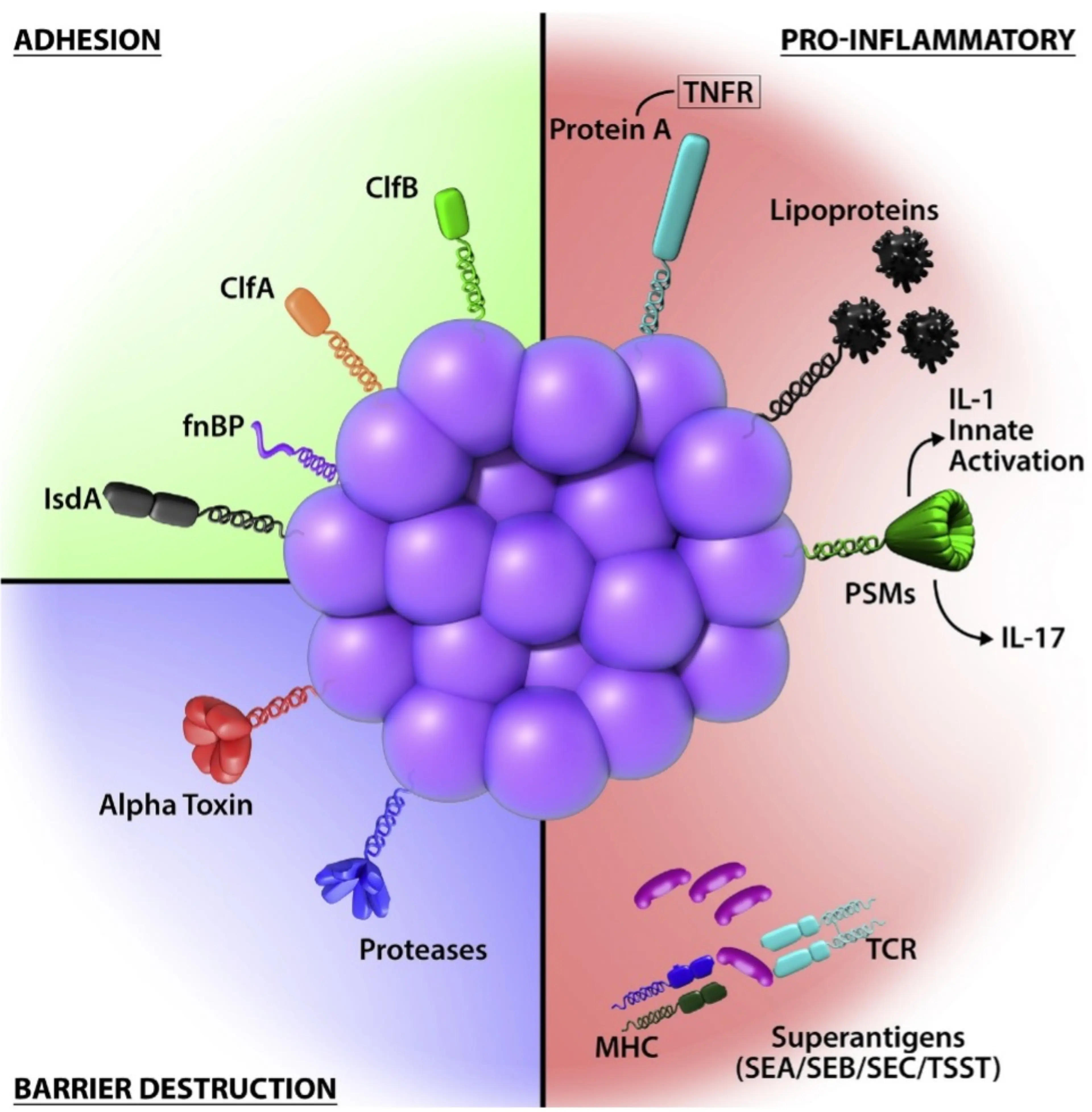
Figure 5: Mechanisms facilitating adhesion, epidermal dysfunction, and proinflammatory mechanisms by S. aureus5
- Langan SM, et al. Lancet 2020; 396: 345–60.
- Weidinger S, et al. Nat Rev Dis Primers. 2018;4(1):1.
- Kim BG, et al. Allergy Asthma Immunol Res. 2018;10(3):207-215.
- Cevikbas F, et al. Physiol Rev. 2020;100(3):945-982.
- Paller A, et al. J Allergy Clin Immunol. 2019;143(1):26-35.
MAT-BH-2600009