- Article
- Source: Campus Sanofi
- 17 Sep 2025
AD Burden on Patients
Understanding the Burden of Atopic Dermatitis on Patients
Atopic dermatitis (AD) places a significant burden on patients’ lives, impacting much more than just the skin. For millions worldwide, AD causes
ongoing discomfort, affects mental and social well-being, and leads to both direct and indirect economic challenges.1-3
Chronic Symptoms of Atopic Dermatitis
Chronic atopic dermatitis is marked by a persistent and evolving set of symptoms that can severely impact patients’ daily lives. These symptoms often
last for months or years and are characterized by both their physical appearance and their impact on comfort and function.3
Key Chronic Symptoms
The skin becomes thickened and leathery as a result of repeated scratching and rubbing. This is a classic sign of chronic AD, typically seen in areas that are frequently irritated.4
Intense, chronic itch remains the most burdensome symptom, often leading to ongoing scratching, disturbed sleep, and further skin damage.4,5
The skin is constantly dry, flaky, and rough in texture. This dryness affects both affected lesions and surrounding areas, exacerbating irritation and itch.4,5,7
Over time, affected skin may darken (hyperpigmentation) or lighten (hypopigmentation), especially at sites of repeated inflammation and scratching. Chronic lesions may appear darker or lighter in people with different skin tones.5,6,9
Chronic patches or plaques may become firm, thick, and show exaggerated skin lines (lichenification). These lesions can persist for long periods and are less likely to ooze compared to acute flares.4,5
The chronic dryness can lead to painful skin cracks (fissures), especially on the hands, feet, or behind the ears, increasing infection risk.5,7
Frequent outbreaks of Staphylococcus aureus and viral infections such as herpes simplex are more likely due to ongoing skin barrier breakdown and scratching.8
Features like ichthyosis (generalized scaling), palmar hyperlinearity (exaggerated skin lines on the palms), and other subtle changes may be noted in longstanding disease.4
Chronic atopic dermatitis symptoms not only cause physical discomfort but are also associated with substantial psychosocial and quality-of-life
burdens, highlighting the need for comprehensive, ongoing management.5,7,8
Impact of Atopic Dermatitis on Quality of Life
Atopic dermatitis (AD) goes far beyond the skin, reducing quality of life (QoL) in profound and lasting ways for both patients and their families.10,11
Physical and Emotional Burden
-
Persistent itch and discomfort are the most distressing symptoms, reported as severe by most patients, leading to constant scratching,
pain, and skin damage.10,11,15
-
Sleep disturbances are common, with poor sleep quality affecting up to 92% of patients, resulting in daytime fatigue, impaired
concentration, and decreased school or work performance.10,11
-
Emotional consequences such as depression, anxiety, embarrassment, and low self-esteem are frequently reported, especially in those
with severe or visible disease.10,15,16
- Over half of adult AD patients report a moderate to extremely large impact on their overall quality of life.12,13,16
- In children and adolescents, AD can lead to social isolation, bullying, and fewer friendships, especially for those with severe disease.11
Social and Daily Functioning
- Social withdrawal and limitations: The visibility of lesions and constant need for treatment cause many patients and families to avoid social activities or alter their routines.10,11
- Academic and work impact: Nearly one-third of adults with AD have experienced challenges at school or work, and 14% believe their academic or career advancement has been hindered by their disease.11
- Family burden: Caregivers—especially parents of children with AD—report significant stress, time commitment for treatments, and emotional distress related to their child’s condition.11,13,15
Severity Matters
The impact of AD on all quality of life measures increases sharply with disease severity. In studies using quality of life indexes, children
and adults with moderate-to-severe AD report a “very large” or “extremely large” effect on daily life more than twice as often as those
with mild disease.12-14,16
Long-term and Lifelong Impact
- Severe, uncontrolled AD from childhood into adulthood leads to enduring difficulties in school, work, and forming social relationships, sometimes even influencing career paths.10
- The burden can accumulate over a lifetime, contributing to poorer long-term health and social outcomes.10,11
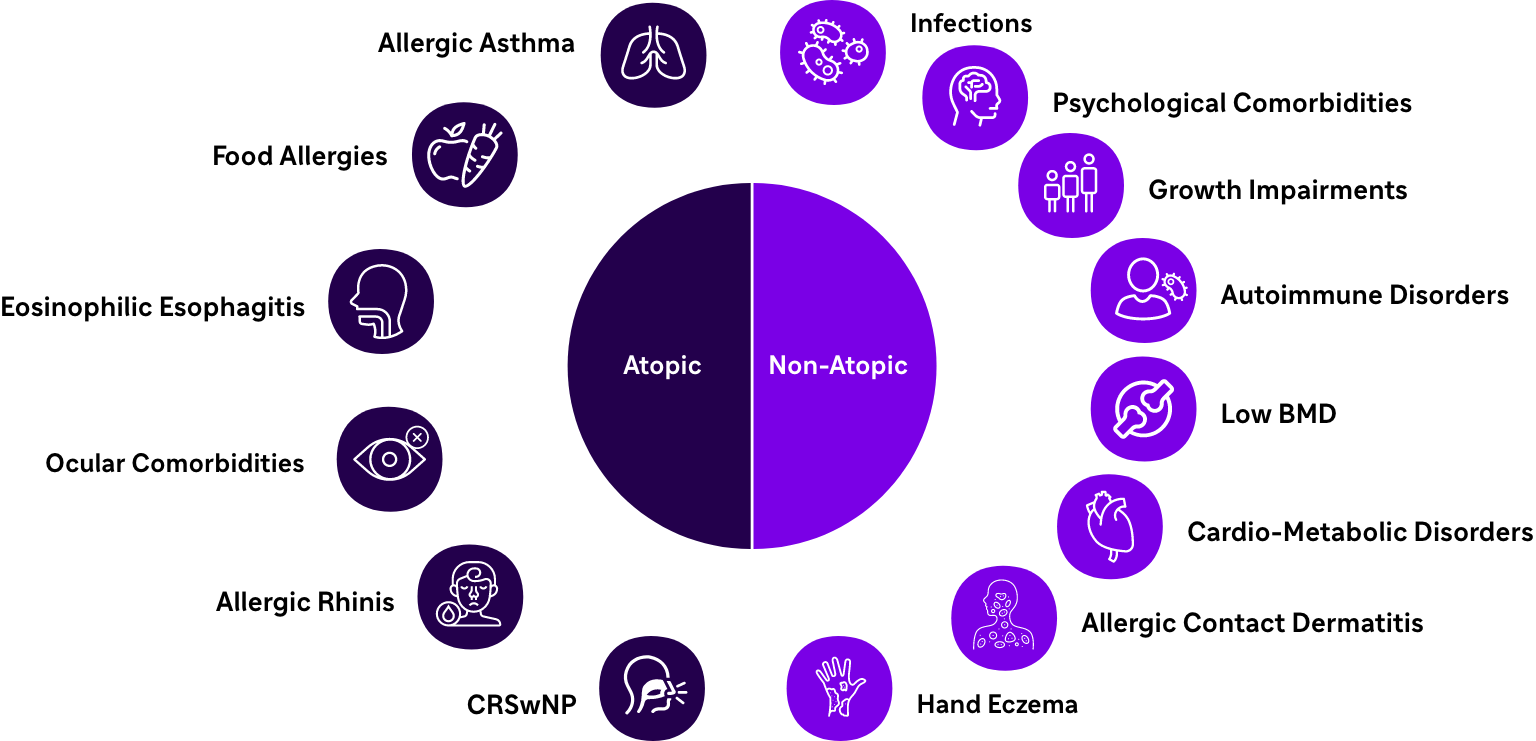
Comorbidities17-22:
Economic Burden of Atopic Dermatitis on Patients
Atopic dermatitis (AD) imposes a substantial financial and productivity burden on patients, families, and society. The costs are both direct—arising
from medical care—and indirect, resulting from reduced productivity and impaired daily functioning.
Direct Costs
The impact of AD on all quality of life measures increases sharply with disease severity. In studies using quality of life indexes, children
and adults with moderate-to-severe AD report a “very large” or “extremely large” effect on daily life more than twice as often as those
with mild disease.12-14,16
- Medical Expenses: Patients with AD face significantly higher health care expenditures than those without AD. In adults, annual direct health care costs can be nearly $5,000 higher per patient, encompassing physician visits, hospitalization, prescription medications (including costly newer therapies), and outpatient services.23
- Treatment-Related Costs: Frequent clinic appointments, management of complications, and long-term use of topical or systemic therapies further increase financial strain.24
- Out-of-Pocket Expenses: Patients and families often pay for moisturizers, special skin care products, specific clothing or bedding, and transportation to healthcare providers.23,24
Indirect Costs
Lost Productivity: AD leads to increased absenteeism and loss of workdays. Adults with AD report more missed work or school days and higher utilization of short-term disability benefits compared to the general population.23
Reduced Work Capacity: The physical discomfort and sleep disturbances from AD negatively impact concentration, work efficiency,
and even career choices or advancement.23
Family Burden: Beyond the patient, family members may incur additional costs for caregiving and experience productivity loss due to
time devoted to ongoing care needs.25
Healthcare utilization: Patients with AD have increased physician office visits and outpatient pharmacy use.26
Severity dependence: Economic burden intensifies with increasing severity of AD, leading to more interventions, treatment changes,
and lost workdays.26
1. https://jamanetwork.com/journals/jamadermatology/fullarticle/2793426
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC9674816/
3. https://www.liebertpub.com/doi/10.1089/derm.2022.29015.jsi
4. https://www.msdmanuals.com/professional/dermatologic-disorders/dermatitis/atopic-dermatitis-eczema
5. https://nationaleczema.org/types-of-eczema/atopic-dermatitis/
6. https://www.niams.nih.gov/health-topics/atopic-dermatitis
7. https://www.en.eucerin-me.com/skin-concerns/atopic-dermatitis/on-the-face
8. https://www.dexeryl.com/en/your-skin/atopic-dermatitis/eczema-symptoms
9. https://www.nhs.uk/conditions/atopic-eczema/
10. https://pmc.ncbi.nlm.nih.gov/articles/PMC8163918/
11. https://nationaleczema.org/eczema-facts/
12. https://www.actasdermo.org/es-impact-atopic-dermatitis-on-health-related-articulo-S1578219012003563
13. https://pmc.ncbi.nlm.nih.gov/articles/PMC10211415/
14. https://www.mdpi.com/2077-0383/13/6/1700
15. https://skinallergyjournal.com/impact-of-atopic-dermatitis-on-quality-of-life-in-children-and-their-families-a-tertiary-care-hospital-based-study-from-northern-india/
16. https://medicaljournalssweden.se/actadv/article/view/1692/3513
17. Hong CH, et al. J Cutan Med Surg. 2019;23(5_suppl):12S-18S.
18. Avena-Woods C. Am J Manag Care. 2017;23(8 Suppl):S115-S123.
19. Silverberg JI. Ann Allergy Asthma Immunol. 2019;123(2):144-151.
20. Weidinger S, et al. Nat Rev Dis Primers. 2018;4(1):1.
21. Canonica GW, et al. Respir Med. 2020;166:105947.
22. Zander N, et al. J Eur Acad Dermatol Venereol. 2020;34(1):135-41.
23. https://www.jmcp.org/doi/10.18553/jmcp.2021.27.10.1416
24. https://pubmed.ncbi.nlm.nih.gov/29063433/
25. https://www.nature.com/articles/s41598-025-91896-y
26. https://www.sciencedirect.com/science/article/pii/S0001731024006021
MAT-KW-250016-V1.0-04/2025