- Hulpmiddelen
- Bron: Campus Sanofi
- 7 mrt 2025
Atopic Dermatitis Control Tool (ADCT)

Introducing ADCT
- Atopic Dermatitis Control Tool (ADCT) – a validated, brief and easily scored tool
- Six concise questions to evaluate all dimensions of atopic dermatitis (AD) control identified as relevant by patients and clinicians
- ADCT can be self-assessed by patients or used in routine consultations
- ADCT is designed to help facilitate meaningful patient–physician discussion on control of AD in every day clinical practice, enabling improvements in disease monitoring
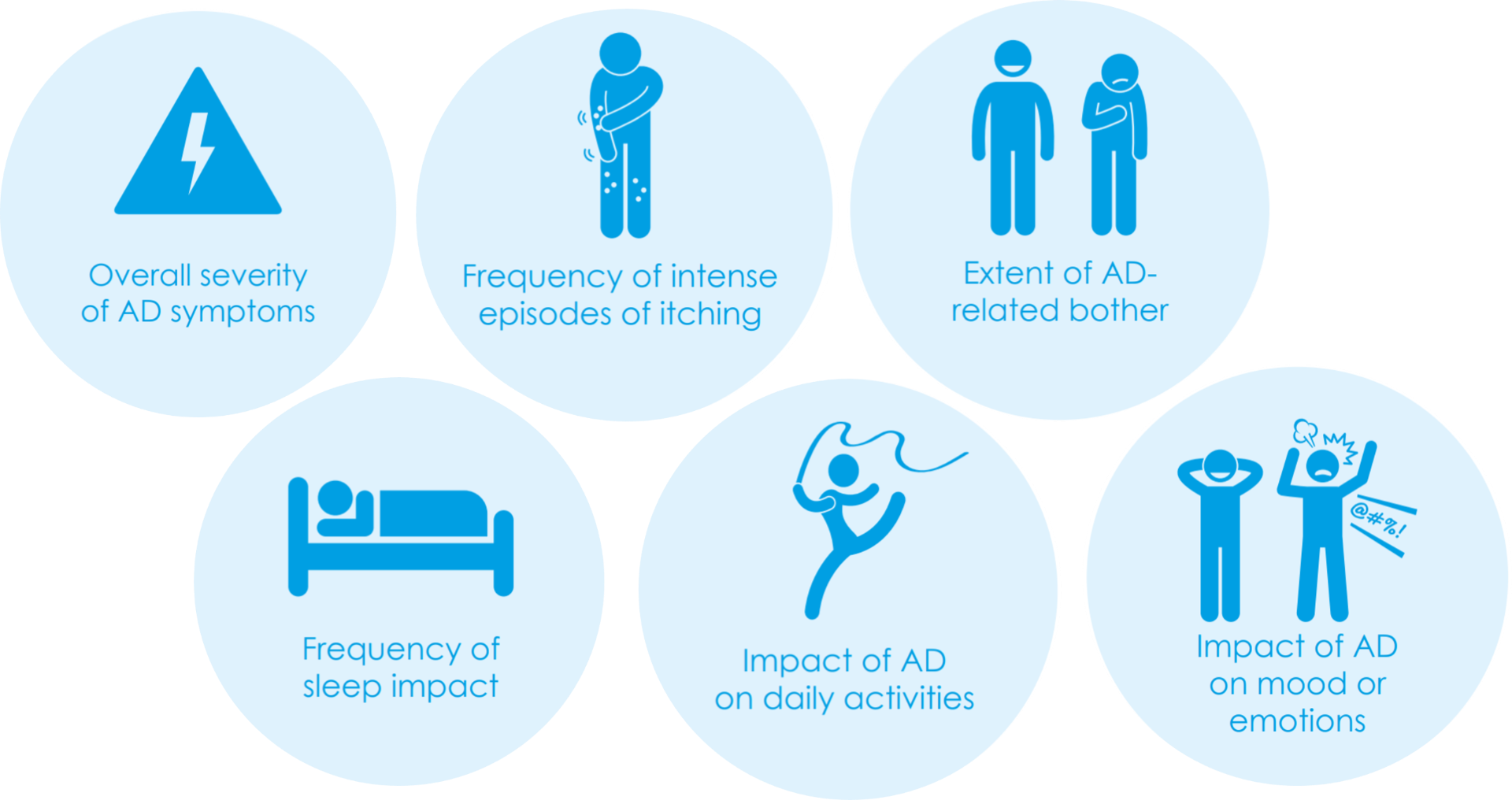
Development of ADCT involved interviews with patients as well as physicians. Six main areas were found critical in assessing the multi-dimensional aspects of disease control over the course of a week, and form the basis of ADCT:
ADCT Validation
ADCT was rigorously tested with 270 US patients who were clinically diagnosed with AD by a healthcare professional, and were using a prescription treatment for AD within the past 6 months (not including oral antihistamines or oral antibiotics)1. Two studies confirmed that ADCT is a valid and reliable tool for assessing AD control and that it can be used to detect change of disease activity in a person over time 1,2.
ADCT is recommended by HOME3
ADCT has been recommended by the Harmonising Outcome Measures for Eczema (HOME) initiative as one of the core instruments for assessing long-term control in atopic dermatitis.3
HOME is a global initiative of healthcare professionals, patients, carers, regulatory bodies, journal editors and the pharmaceutical industry to develop a consensus-based core outcome set for clinical trials. The core outcome set of parameters that are recommended by HOME to be measured in all clinical trials comprises:
- Clinician-reported signs of atopic dermatitis
Recommended tool: Eczema Area and Severity Index (EASI)
- Patient-reported symptoms
Recommended tools: Patient-Oriented Eczema Measure (POEM) and Numerical Rating Scale (NRS) 11 (for peak itch over past 24h)
- Quality of Life
Recommended tools: Dermatology Life Quality Index (DLQI), Children Dermatology Life Quality Index (CDLQI), Infant Dermatology Life Quality Index (IDQoL)
- Long-term control of atopic dermatitis
Recommended tools: Recap of atopic eczema (RECAP) and Atopic Dermatitis Control Tool (ADCT)
ADCT Scoring Instructions
To use ADCT correctly, your patient must answer all six ADCT questions by selecting the most appropriate answer.
| 0 points | 1 point | 2 points | 3 points | 4 points | |
|---|---|---|---|---|---|
|
1. Over the last week, how would you rate your eczema-related symptoms? | None | Mild | Moderate | Severe | Very Severe |
|
2. Over the last week, how many days did you have intense episodes of itching because of your eczema? | Not at all | 1-2 days | 3-4 days | 5-6 days | Everyday |
|
3. Over the last week, how bothered have you been by your eczema? | Not at all | A little | Moderately | Very | Extremely |
|
4. Over the last week, how many nights did you have trouble falling or staying asleep because of your eczema? | No nights | 1-2 nights | 3-4 nights | 5-6 nights | Every night |
|
5. Over the last week, how much did your eczema affect your daily activities? | Not at all | A little | Moderately | A lot | Extremely |
|
6. Over the last week, how much did your eczema affect your mood or emotions? | Not at all | A little | Moderately | A lot | Extremely |
Calculating the ADCT Score
Step 1: Each ADCT question is scored 0–4 points, as shown in the table above
Step 2: The sum of the scores from all six ADCT questions forms the ADCT total score The minimum score is 0, the maximum score is 24
Interpreting the ADCT score
Point in time control status
A higher score indicates lower AD control
A patient's AD may not be well controlled if:
- The ADCT total score is at least 7 points
Changes in control status over time
A change of 5 points in the threshold for meaningful within person change
- Decrease of 5 points or more: indication of clinically relevant improvement of AD control
- Increase of 5 points or more: indication of clinically relevant worsening of AD control
Point in time control status
A higher score indicates lower AD control
A patient's AD may not be well controlled if:
- The ADCT total score is at least 7 points
Changes in control status over time
A change of 5 points in the threshold for meaningful within person change
- Decrease of 5 points or more: indication of clinically relevant improvement of AD control
- Increase of 5 points or more: indication of clinically relevant worsening of AD control
Recommendations for using ADCT in clinical practice
Your patient’s AD may not be well controlled if:
- Their ADCT total score is at least 7 points
OR
- Their ADCT total score has increased by 5 points or more since they last used ADCT
If you are concerned that your patient’s AD is not well controlled, you might want to initiate further conversations about optimal management of their AD.
Assess atopic dermatitis with your patients
Ask to take the ADCT and POEM tests onilne:
Atopic Dermatitis Control Test (ADCT)
Atopic dermatitis, a type of eczema, may be affecting your patient’s life in more ways than you know.
The ADCT gives a measure of how controlled your patient’s eczema is. Use these 6 concise questions to evaluate all dimensions of atopic dermatitis control.
Development of ADCT involved literature review as well as interviews with patients and physicians, and was funded by Sanofi and Regeneron.
Neem contact op

Referenties
-
David M Pariser et al., Evaluating patient-perceived control of atopic dermatitis: design, validation, and scoring of the Atopic Dermatitis Control Tool (ADCT). Current Medical Research and Opinion 2019. DOI: 10.1080/03007995.2019.1699516
-
Eric Simpson et al.,. Validation of the Atopic Dermatitis Control Tool (ADCT©) using a longitudinal survey of biologic-treated patients with atopic dermatitis. BMC Dermatology 2019;19:15. DOI: 10.1186/s12895-019-0095-3
-
http://www.homeforeczema.org/research/long-term-control.aspx. Accessed November 2024
MAT-BE-2401077 v1.0 1/25