- Artikel
- Bron: Campus Sanofi
- 25 mrt 2025
Need to identify risk of developing autoimmune type 1 diabetes? Test for autoantibodies!

Key takeaway
Why screen for autoantibodies?
Autoimmune T1D is associated with the appearance of autoantibodies many months or years before symptom onset.1 Decline in beta-cell function occurs in three distinct stages and by the time clinical symptoms manifest, significant beta-cell loss has typically occurred.1,2 Screening for autoantibodies is important for early detection of beta-cell destruction and provides patients/caregivers with opportunity to access healthcare providers to help them prepare and develop skills for better management of T1D.2,5,6 The autoantibodies detected in autoimmune T1D include:1,2
- Glutamic acid decarboxylase antibodies (GADA)
- Insulinoma-associated-2 autoantibodies (IA-2A)
- Insulin autoantibodies (IAA)
- Zinc transporter 8 autoantibodies (ZnT8A)
Stages of autoimmune T1D depicting progressing beta-cell function decline2








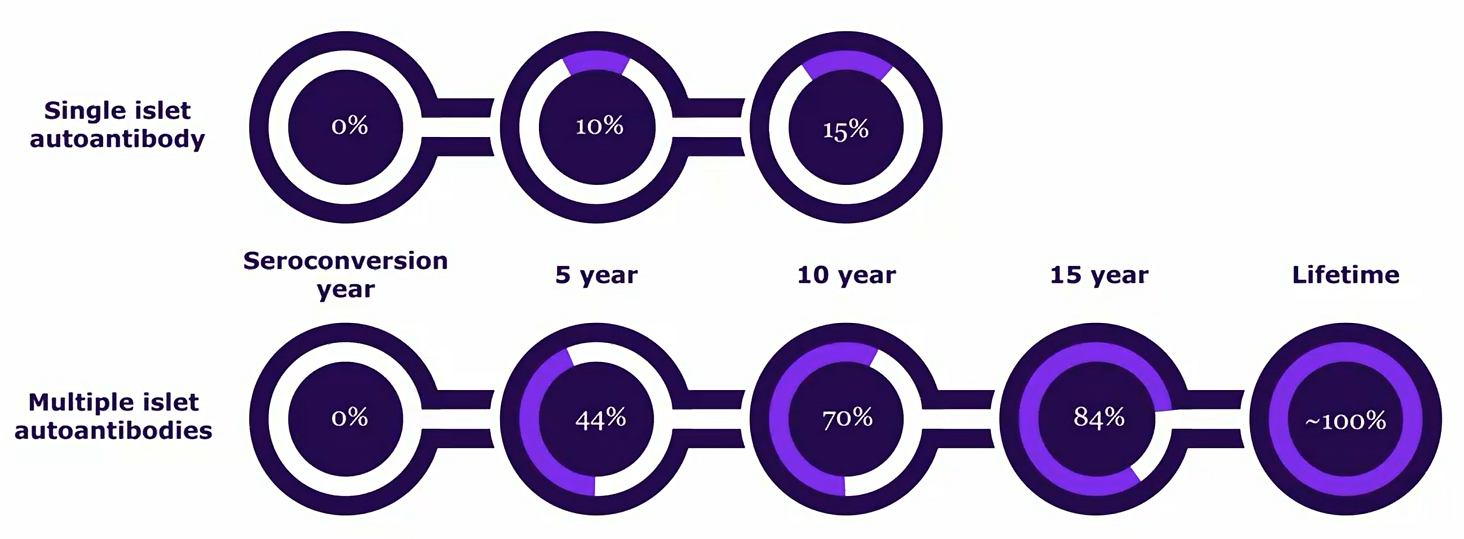
How the presence of islet autoantibody determines risk of T1D
The number of detectable autoantibodies through screening correlates with risk of developing autoimmune T1D.2,6 The majority of individuals with a single autoantibody do not progress to autoimmune T1D.7 However, presence of two or more autoantibodies increases the risk of progression to clinical T1D to 70% over 10 years and 100% over lifetime.6
Risk of progression to autoimmune T1D after seroconversion to islet autoantibody positivity6
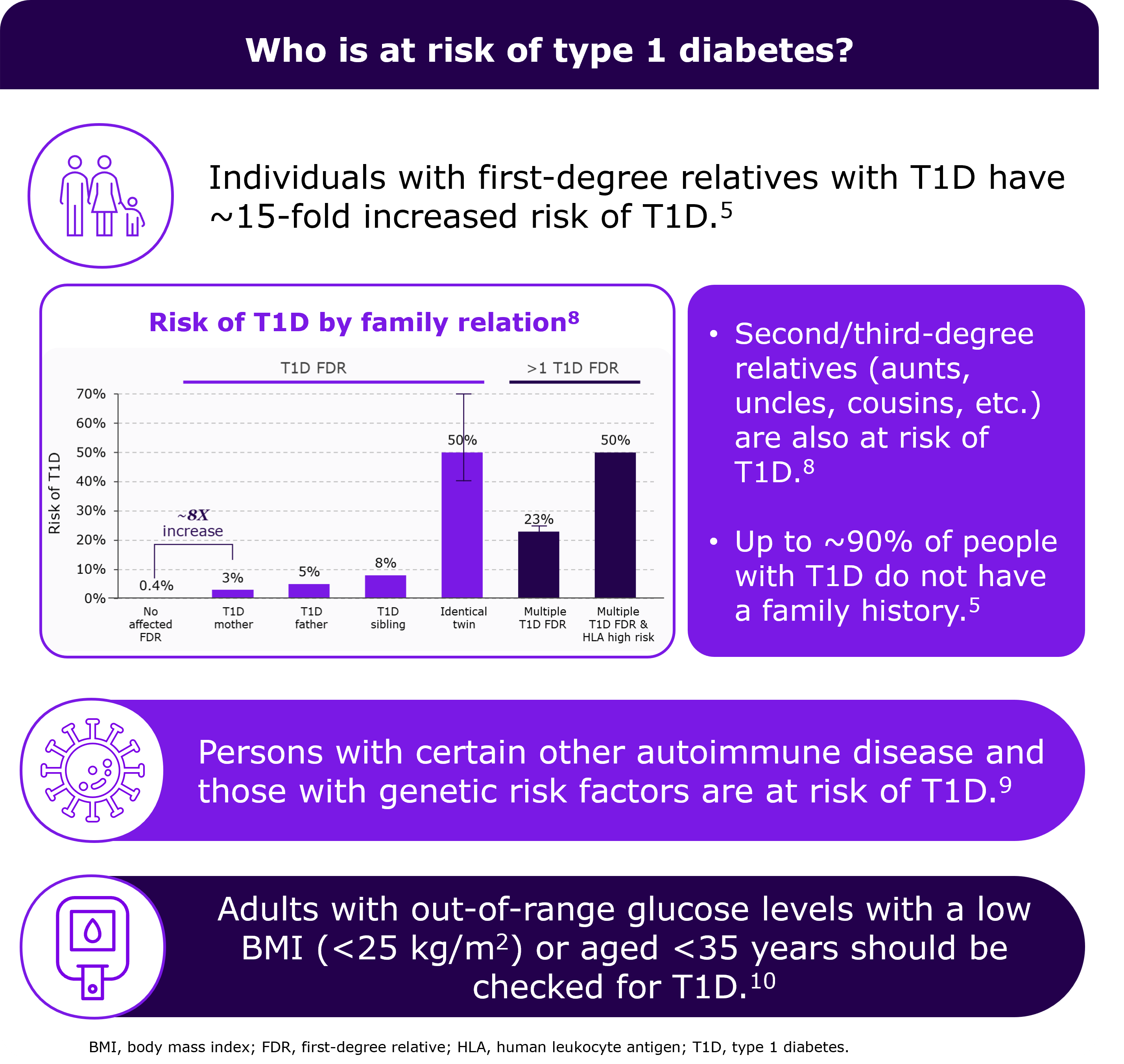
Who should be screened for islet autoantibodies?
Individuals with a family history of T1D are at greater risk of developing the disease, with up to a 15-fold increased risk if a first-degree relative has T1D.5 Additionally, individuals with certain other autoimmune diseases (e.g. celiac disease and autoimmune thyroiditis) and adults with out-of-range glucose levels with a low BMI (<25 kg/m2) or aged <35 years are also likely to develop T1D.9,10
Click here to visit BR1DGE – a global medical education program organized by Sanofi – to learn more about who might benefit from screening for autoantibodies –
Please note that clicking this link will direct you to another website.
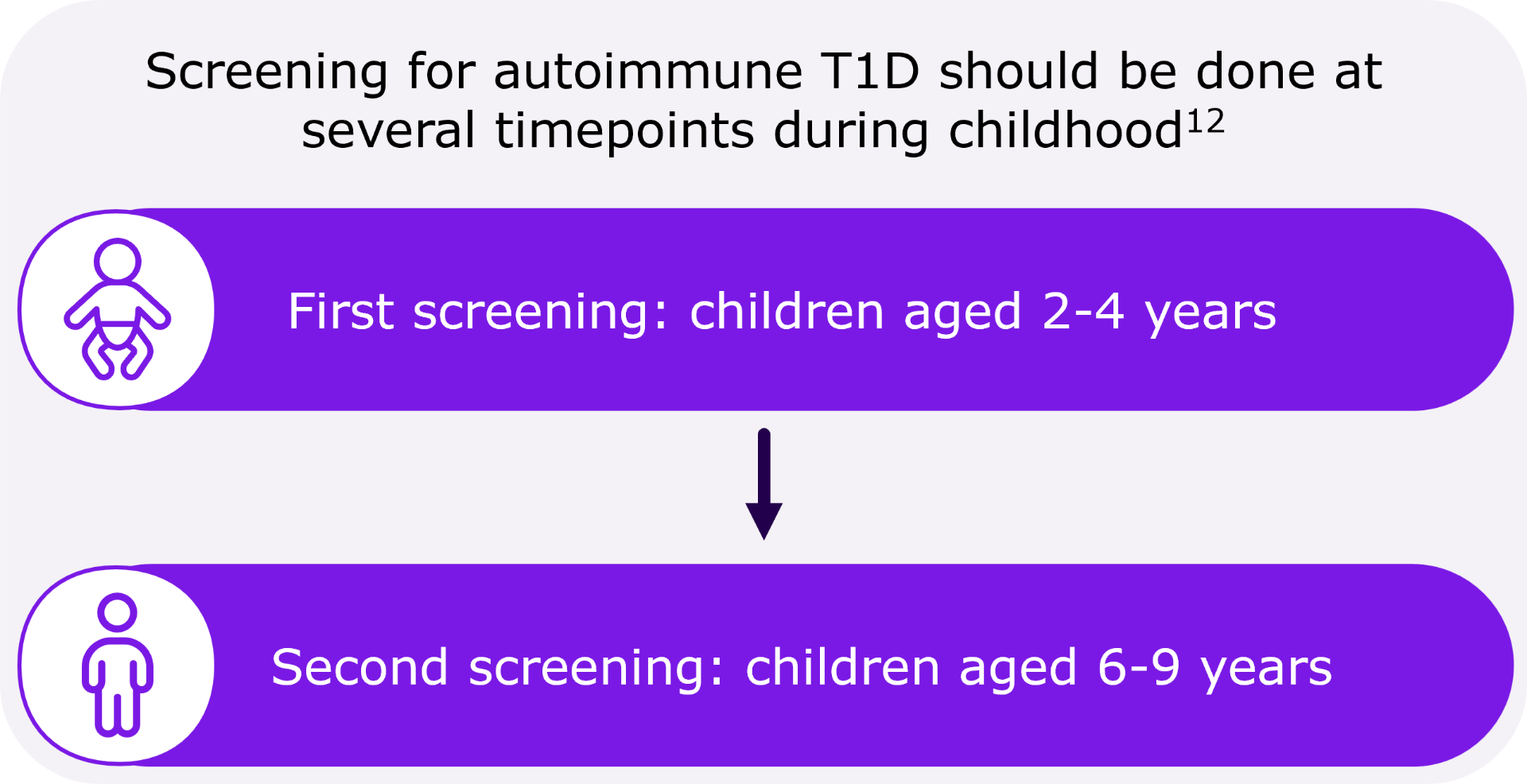
What is the right age for screening for autoimmune T1D?
Although T1D can manifest at any age, it most commonly occurs in children, teenagers, or young adults.1,11 Autoantibodies often emerge before the age of 6, even in cases where T1D is diagnosed much later in childhood. Screening for islet autoantibodies at ages of 2 and 6 has proven to be sensitive and efficient in predicting autoimmune T1D.12
What are the benefits of screening for autoimmune T1D?
Screening shows that approximately 95% of relatives of individuals with T1D test negative for autoantibodies, which can provide reassurance, especially to families with an affected member.5
In individuals who test positive for autoantibodies, screening leads to early detection of autoimmune T1D, which in turn: 6,14-16
- Can prevent diabetes ketoacidosis, a potentially life-threatening complication of diabetes.
- Provide preparation time to individuals and their caregivers to develop skills to manage T1D.
- Enable access to healthcare to provide ongoing education and monitoring.
Click here to visit BR1DGE – a global medical education program organized by Sanofi – to learn more about metabolic monitoring in individuals with presymptomatic autoimmune T1D –
Please note that clicking this link will direct you to another website.
-
Katsarou A et al. (2017) Nat Rev Dis Primers. A1063 17016
-
Insel RA et al. (2015) Diabetes Care. 38(10),pp.1964-1974
-
Tiberti et al. (2011) Clin Exp Immunol. 166(3) pp.317-324
-
Cortez et al. (2020) PLoS One. 15(11), pub. Nov 13 2020 e0242049
-
Sims EK, et al. (2022) Diabetes 71(4) 610-623
-
Simmons KM ad Sims EK (2024) J Clin Endocrinol Metab. 108(12),pp.3067-3079
-
DiMeglio LA, et al. (2018) Lancet. 391(10138) - 2449-2462
-
Ziegler A-G and Nepom GT (2010) Immunity 32(4),pp.468-78
-
Mäkimattila S et al. (2020) Diabetes Care, May 43(5),pp.1041-1047
-
American Diabetes Association (2024) Standards of care in diabetes—2024. Diabetes Care. 47(suppl 1),pp.1-S321
-
You W-P and Henneberg M (2016) BMJ Open Diabetes Res Care 4(1) - e000161
-
Ghalwash M et al. (2022) Lancet Diabetes Endocrinol. 10(8),pp.589-596
-
Greenbaum CJ (2021) Diabetes. 70(5) 1029-1037
-
Nakhla M, et al. (2021) JAMA Pediatr. 175(5) 518-520
-
Hummel et al. (2023) Diabetologia, Vol. 66, pp. 1633–1642
-
Smith LB, et al. Pediatr Diabetes. 2018 19(5) 1025-1033
-
El Sayed NA et al. Diabetes Care 2023 46 (Suppl. 1) S19–S40
Neem contact op

MAT-BE-2500177-1.0-02/2025



